GYA’s 2023 International Conference for Young Scientists
Thursday, 6th June 2023

At the “GYA’s 2023 International Conference for Young Scientists” in Kigali, Rwanda, I had the privilege of discussing a critical issue: achieving equitable and effective vaccine distribution in low- and middle-income countries (LMICs). Some of the insights shared includes:
Global Vaccine Acceptance – where Europe and the United States seeing rates around 70-75%. In Africa, rates range from 30% to 60%, highlighting the need for targeted strategies to increase uptake.
Demographic Disparities – Despite gender differences in vaccine acceptance being minimal, younger adults (18-35) in Europe and the U.S. show lower acceptance rates than older groups. This underscores the need for outreach and education campaigns aimed at younger populations.
Africa faces unique challenges, but Rwanda stands out with over 70% acceptance due to strong health prioritization and community engagement. This success provides a model for other LMICs.
The disparity in vaccine access between high-income countries and LMICs is stark. High-income countries have secured more doses, leaving LMICs at a disadvantage. Collaboration, technology transfer, and initiatives like COVAX are vital to address this imbalance.
Overcoming Vaccine Hesitancy – Combatting vaccine hesitancy and misinformation in LMICs requires strengthening health systems, training healthcare workers, and fostering community trust. Rwanda’s approach offers valuable lessons for other nations.
Achieving equitable vaccine distribution in LMICs demands collective action and a commitment to fairness. By addressing demographic disparities and learning from successful models, we can build a resilient global healthcare system and ensure no one is left behind.
2024 Global Health Policy Forum
Thursday 27th April 2023

I had the honor of participating in the Partnership for Quality Medical Donation’s annual Global Health Policy Forum in Paris, where I gave a Keynote Speech on the Topic ““Importance of Health Equity in a World of Rapid Climate Change” and later joined a Panel discussion where I addressed multifaceted issues that are shaping the post COVID-19 pandemic era. I highlighted how COVID-19 has amplified existing socio-economic disparities rather than creating them from scratch – Talked about Rwanda’s innovative contact tracing methods and advocating for a regional collaborative approach towards creating localized solutions that specifically addresses our needs and challenges.
Central to my address was the call for equitable leadership in global health, necessitating both a decolonization of practices and fostering of solidarity – in majority of the instances, the crisis is not due to scarcity but rather an uneven distribution. The crucial Global Health equity agenda, intertwined with national safety and health system robustness, was a core theme, while the need for innovative education to produce future leaders who champion evidence-based and equitable solutions stood out as pivotal. The forum embodied the spirit of collaborative discourse, paving the way for an equitable and resilient future in global health.
Guest Lecture: Georgetown School of Foreign Services (Dr. Agnes Binagwaho)
Thursday, 13th April 2023

Delivered a guest lecture at Georgetown School of Foreign Service, where I shed light on pivotal aspects of healthcare leadership and financing. I discussed the intricate process of budget prioritization that is essential for effective healthcare delivery while emphasizing the delicate balance of managing donor priorities alongside the needs of the country, showcasing Rwanda’s innovative approach to harmonizing these agendas.
Delved into the Five Principles of the Paris Declaration on Aid Effectiveness (2005) as benchmark and the The Accra Agenda for Action (2008) elaborating donors’ commitment to “use country systems as the first option for aid programs in support of activities managed by the public sector.”. I gave an overview of the complex landscape of health financing, both within Rwanda and globally, underscoring the significance of understanding financial flows within the healthcare sector. A focal point of my lecture was the journey Rwanda embarked upon to achieve universal healthcare coverage – I accentuated the significance of accessibility enhancements, shedding light on Rwanda’s groundbreaking “Mituweli” Health Insurance Solution – a model emphasizing inclusivity, equity, and scientific holistic approaches. As we look to the future, I believe these insights can guide us towards building stronger, more resilient healthcare systems globally.
C20 Integrated Holistic Health Summit
7th – 9th of April 2023
In my keynote speech at the C20 Integrated Holistic Health Summit, that took place from 7th-9th of April 2023 at the Amrita Hospitals convention center in India, I emphasized the importance of embracing a comprehensive and integrated approach to healthcare. I reminded all that true well-being encompasses not only physical health but also mental, emotional, and social dimensions. Accessible and holistic care must be a universal right, achievable through collaborative efforts among governments, healthcare institutions, researchers, and communities. I believe in our ability to drive positive change and make holistic healthcare the norm while extending my gratitude to the summit’s organizers for facilitating this crucial global dialogue.
“We are focused on access to better holistic integrated care, and we are going with hope because we know what we can do to do better.” – Said Prof.Agnes Binagwaho
China Medical Board Foundation Equity Initiative Annual Forum
February 3, 2023

I was invited by the China Medical Board Foundation to take part of the Equity Initiative Annual Forum, where I shared critical moments in my leadership journey and some advice for the aspiring young change-makers in the field of health. I presented my journey in global health, best described by my contribution to the rebuilding of Rwanda’s health sector. Together we reviewed, the history of Rwanda, focusing on the 1994 Genocide Against the Tutsi, then we discussed some strategies used to strengthen the health system and improve health outcome such as building trust for health systems. Lastly, I also presented my work in health science education, using the University of Global Health Equity as an example.
Prince Mahidol Award Conference Plenary Session
January 28, 2023

I was invited for the Prince Mahidol Conference which is themed on : “Setting a New Health Agenda – at the Nexus of Climate Change, Environment and Biodiversity” as a moderator for a plenary session. Prince Mahidol Award Conference is to bring together leading public health leaders and stakeholders from around the world to discuss high priority global health issues, summarize findings and propose concrete solutions and recommendations. The session aimed to provide the opportunity for panelists to critically reflect on priority actions needed to address the current climate, biodiversity and health crises. Examples of using the youth, and other local governance examples were provided on how to address these issues.
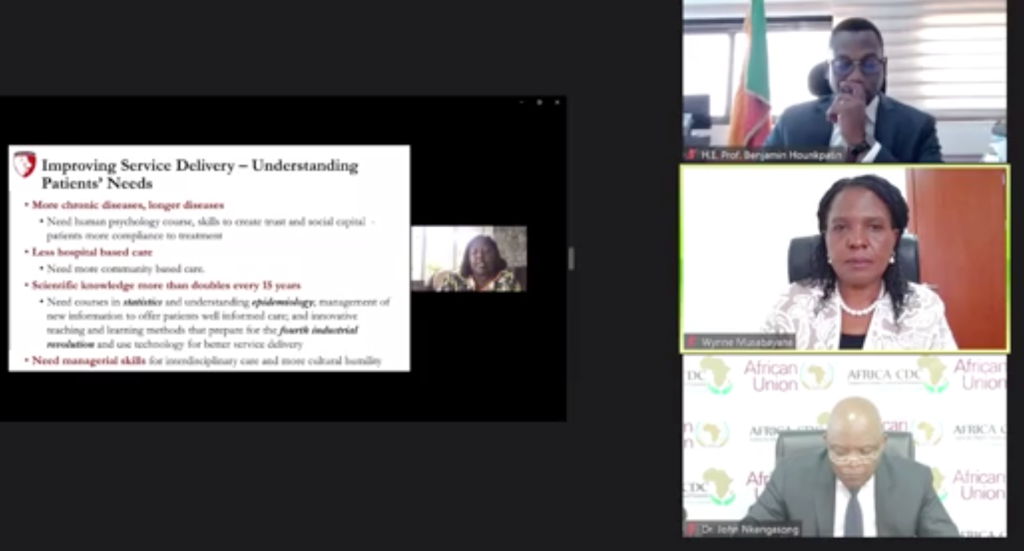
CPHIA – Track 8 Plenary: Plenary: A Renewed Focus on Africa’s Major Infectious Diseases: HIV, TB, Malaria and NTDs
December 14, 2022

For CPHIA, they were 9 tracks and I participated in Track 8, which focused on infectious diseases. I presented on the “The State of HIV in Africa: A presentation describing current epidemiology of HIV, impact of SARS-CoV-2, and strategies for the future”. In the presentation, I discussed progress on the journey towards the 90%(diagnosed)-90% (on treatment)-90% (virally suppressed) target where only 5 countries have achieved this in Africa, which includes Rwanda; I also presented COVID-19 related demand and supply side interruptions and the response strategies; provided a way forward to reduce morbidity and mortality from HIV/AIDS such as using implementation research to understand the needs and best solutions fit to the context.
2nd Conference on Public Health in Africa Opening Ceremony
December 13, 2022

As the Co-Chair of the International Conference on Public Health in Africa, I took part of the opening ceremony where I gave opening remarks. This conference is a platform for health leaders to discuss the health issues on the continent and it is the second of its kind. This was first in person in conference and it happened in Kigali, Rwanda.
“The 1st Inaugural International Conference on Public Health in Africa was an extraordinary meeting that came at an opportune time to evaluate actions of the previous two years and forge a way forward, leveraging successes and addressing obstacles to ensure the health security of the African continent. It brought together renowned public health experts from across the continent, including top researchers, senior and junior scientists, clinicians, political leaders and a global audience of over 12,000 participants. Participants discussed important topics within the field of public health in Africa. This much-needed scientific platform – in the midst of the COVID-19 pandemic – empowered Africans to own the continent’s public health narrative, forge a strong way forward to improve African population health outcomes. Most importantly, this conference highlighted the need for a New Public Health Order in Africa that is characterized by a strengthened Africa CDC and national public health institutions (NPHIs); local production of vaccines, therapeutics, and diagnostics; investment in public health workforce and leadership programs; and respectful partnerships.”
Watch Full Ceremony: https://www.youtube.com/watch?v=ibAjTXHIbqI
CPHIA- Child Depression Screening Tool Multi-country Study Dissemination Workshop
December 12, 2022
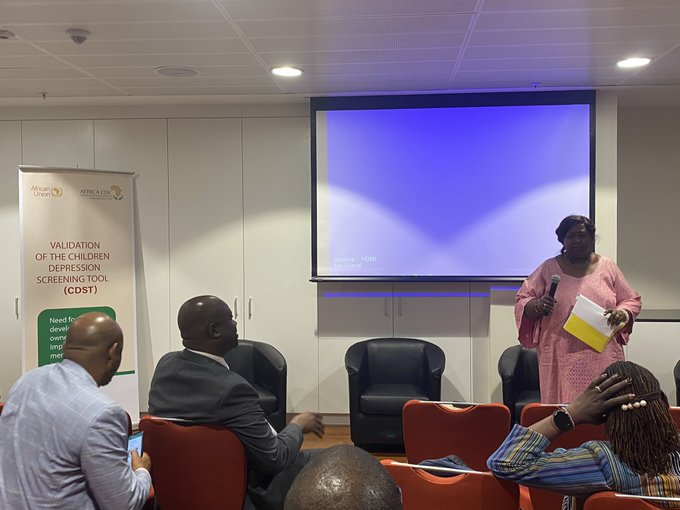
As a continuum of the Conference public health in Africa, I took part of the dissemination workshop on a child depression screening tool I developed, that was validated in Rwanda already. The tool is a free and open-source tool that can be used by non-mental health specialists such as nurses. It was validated in Senegal and South Africa and it was used on children and adolescents with chronic diseases and in different settings such as schools, refugee camps and health facilities.
There are many benefits to this tool “First, this will help improve access to mental health services for children, that are already facing hardship and difficulties because of their medical condition and their social-economic status, thus allowing better health outcomes for them. Second, early detection will help improve prevention and treatment programs for children’s mental health. Third, this will help to monitor and follow-up for these children in the system on a yearly basis and help allocate the necessary resources for where the prevalence or risk appears to be in high proportion. Fourth, financially, this will help reduce health costs for unnecessary diagnostics within health facilities. Fifth, the mental health needs for children that come from low-income families, will be addressed, and supported as well.”
CPHIA- Is primary Health Care the Critical Pathway to Health Security in Africa
December 12, 2022

I was invited in a side event for CPHIA on “Is Primary Health Care the critical pathway to health security in Africa”. I discussed on how the African Union will assist African governments to move into action is as far investing in primary health care for health security is concerned.
“African Union with the technical support of CDC Africa successfully pooled member states’ purchasing power and negotiated with the private and public sectors to secure PPE and vaccines through the Africa Medical Supplies Platform and the Africa Vaccine Acquisition Task Team (AVATT) launched by the chairperson of the African Union”.
CPHIA- National Public Health Institutes on Public Health Workforce Development
December 12, 2022

As co-chair of the conference of Public Health in Africa, together with members of National Public Health Institutes took part of a conversation on public health workforce development. In this session, I co-chaired with Dr. Chikwe, the discussion focused on the challenges of the health workforce in Africa,such as the ratio of physicians per population, training of health care workers and strategies in work were also provided such as the Kofi Annan Global Health Leadership Program.
“As it is reported, that the African continent carries 24% of the global health disease burden yet it constitutes of only to 3% of the global health workforce and among this health workforce body, 41.5 % of them represent health care workers that include nurses, midwives, and community health workers.”
Conference of Public Health in Africa (CPHIA) -” Universal Health Coverage and Children’s Health in Africa: What is working?”
December 12, 2022

I was invited by the Duke Center for Policy Impact in Global Health and Africa CDC Health Economics Program during the Conference on Public Health in Africa (CPHIA) to give a presentation on “Leaving no child behind.” In this talk I discussed how Rwanda has been able to reach marginalized children with coverage. I focused on equity in achieving UHC for children and ‘reaching the last mile’ as Rwanda has had great success in expanding coverage to children and rapidly reducing child mortality. In the lecture, I presented Rwanda’s journey in the reduction of under-five mortality and the strategies used to achieve this exemplar reduction such as the decentralization of the health system.
5th Edition Forum Galien Afrique Panel
December 8, 2022

For the 5th Edition of Forum Galien Afrique, I was invited to take part of a panel on “Role of Women in Science, Technology, Engineering and Mathematics (STEM) and Universal Health Coverage in Africa”. The Prix Galien Africa, awarded for 50 years, is positioned as the Nobel Prize for pharmaceutical innovation. Since 2009, the Galien Foundation has been organizing a scientific forum in the United States in conjunction with the Prix Galien International. In the discussion, I mentioned the role women in STEM play or can play in accelerating Africa’s march towards universal health coverage which is for instance to do research that cater to women’s health issues. Lastly, I also discussed what reforms are needed in the health workforce to attain universal health coverage, including increasing the number of medical schools in Africa.
Financial Times/The Commonwealth Fund Panel: A Path to U.S. Health Equity
December 1, 2022

I was invited by the Financial times to discuss the route to improved and equitable maternal health. he Route to Improved and Equitable Maternal Health bringing in lessons from Rwanda. Since US maternal mortality and morbidity rates are higher than comparable countries and the racial and ethnic disparities in maternal health outcomes are stark, I highlighted on how policies and actions can address avoidable risks using the examples of Rwanda such as bringing care to the community to address gaps in healthcare by building health centers that are 7 minutes away from community members.
The World Academy of Sciences 2022 General Meeting of Fellows & Young Affiliates
November 22, 2022
As a member of the The World Academy of Sciences, I attended 16th TWAS General Meeting. I presented on how to improve science education to advance global health research in LMICs. I discussed changes needed in education to improve the number and quality of the healthcare workforce in LMICs, to improve health outcomes, achieve the SDGs and ultimately improve global health research with a focus on Africa. I provided an overview of challenges facing global health research and education, challenges of the African health workforce, and effects of the COVID-19 pandemic on health education, I discussed the role of universities in achieving the SDGs and provided recommendations and success stories in Africa towards health education strengthening.
Tsinghua University-2022 World Health Forum
November 20, 2022

I was invited by the Tsinghua University for their World Health Forum event to discuss on “Global Experience of Health and Poverty Alleviation” where I used the example of Rwanda. In the discussion, I described the progress that Rwanda has made in the past 28 years in alleviating poverty through an equity approach, by describing the history of the 1994 Genocide Against the Tutsis; presenting Rwanda’s focus on equity across sectors; discussing some of Rwanda’s strategies for poverty alleviation; emphasizing the importance of trust and accountability.
US National Academies Global Forum on Health Professional Education – Implementation Science workshop
November 15, 2022
As a member of National Academies of Science, I was invited to participate in the Global Forum on Innovation in Health Professional Education to give remarks on the “Relevance of Implementation Science in Health Professions Education”. In the presentation, I discussed the importance of implementation science in the health professions education, relating to the needs of an aging population. In the discussion, I presented the need for implementation research; defined implementation research; discussed contextual factors, implementation strategies and outcomes and also present an argument for capacity building in implementation research which is that ” Capacity building in research and specifically in IR helps us to use all known EBIs and implementation strategies, this is key to strengthening health systems and ultimately contributes to economic development; improvements in health improve production capacity which in turn results in economic growth and poverty reduction”.
Africa Health R&D Week
November 11, 2022

I was invited by the AIDS Vaccine Advocacy Coalition (AVAC), International AIDS Vaccine Initiative (IAVI), and the Coalition to Accelerate & Support Prevention Research (CASPR) to take part of the Africa Health R&D week which is a week-long virtual event intended to build on international, continental, and regional advocacy efforts towards increasing domestic financing of research and development as a critical component of health in Africa. In my presentation , I discussed what the colonial legacy looks like within global health today and explore how we can decolonize this field.
Dartmouth University -Governance and Leadership Seminar
November 7,2022
As a Dartmouth Lecturer, I was invited to speak to a group of students taking Governance/Leadership course at the Dartmouth Institute. I gave them a brief overview of my career leadership related to the roles I played in the government & my role at UGHE as vice chancellor, highlighting successes and challenges in leadership. We mainly discussed how the multi-sectorial approach and equity approach is what has led to the successful health systems in Rwanda and in the coordination of programs or organizations created to tackle issues such as HIV or COVID-19, and lastly we also discussed on resource mobilization.
Bielefeld University- Decolonizing Global Health Research
November 2, 2022

I was invited by a German University to speak on decolonizing global health research in the german context, my keynote was aimed at highlighting some of the central aspects – why is decolonization in global health research so important, what is the current status and what is needed, and who is responsible and must play a role.
In the lecture, I examined the colonial legacy within global health and explore why we need to decolonize global health research by discussing the meaning of decolonization; drawing parallels between current global health practices and colonialism; criticizing the current practice of global health; understanding how the western supremacy mindset is cultivated; exploring manifestations of the western supremacy mindset using the example of the global response to COVID-19, evaluating the need to decolonize given the gaps in scientific publications, research, and partnerships for high income countries and LMICs as well as global health education disparities and using the UGHE’s model as an institution working to address this challenge.
African Philanthropist Forum Panel- Closing the Gender Gap
October 25, 2022

I was invited to a panel by the African Philanthropy Forum (APF) which is a strong and vibrant community of partners who through their strategic giving, investments and influence, foster shared prosperity on the African Continent. It was incubated by the Global Philanthropy Forum (GPF), a global network of strategic philanthropists and social investors committed to international causes from 2014 – 2016. In 2017, APF became an independent entity and continues to be an affiliate of the GPF.
Our panel talk was to help acknowledging that both women and men should be engaged as champions of gender equality, will focus specifically on the role that men can play as agents for change, partners, allies, advocates, and gatekeepers of power. In the discussion I highlighted how we can break down unconscious biases, unequal power relations and structures which have placed women at a disadvantage and I mentioned that ” “Equity has to be at the center if you want to fight for #genderequity. It all starts with education, we need to start mentoring that men and women are equal from kindergarten and to the parents as well”. We also touched upon on ways to recruit and engage male champions “As men and women, we must have a common goal to ensure gender equity in all sectors and at all levels” and lastly I also highlighted that to promote all positive contextual factors and fight the obstacles to gender equity & women’s health, we need to get all the help we can from all the communities.
Duke University & University of Global Health Equity(UGHE) Lecture- Equity in Surgical Care
October 20, 2022
I was requested to give a lecture on equity in surgical care and my aim was to transfer knowledge on health equity, inspire an attitude of equity, and lead individuals to introduce equity to their practice. In this lecture I discussed the urgent need to ensure accessible surgical care to all across the globe, with a special focus on Sub-Saharan Africa. I examined the fundamental issues at the center of all health equity conversations and decisions such as double standard for quality health care, I highlighted the burden of surgical diseases and the unmet need in Sub-Saharan Africa such as the fact that 70% of deaths following emergency general surgery happen in LMICs. I also explained what true accompaniment of surgical patients looks like, evaluated the global surgery movement and lastly described the shortage of healthcare professionals and analyzed the UGHE’s model as an institution working to address this challenge.
Women’s Global Leadership Conference
October 13, 2022

I was invited at the Agnes Scott college to discuss on ““Leading Inclusively: Transformative Change Across the Globe.” with Pat Mitchell who is the the editorial director of TEDWomen. In our conversation, I reflected on the value of compassionate leadership, the qualities that define compassionate leadership such as understanding and identifying the vulnerable. I also highlighted on my journey as a pediatrician and the biggest challenges I faced as a woman leader, as an African leader in the global health space.
University of Global Health Equity- French Executive Course Panel
October 7, 2022

As a continuum of “The Digital Health Applied Leadership Program” in french, I took part of a panel on “Understanding the Complexity of Global Health Leadership: Leaders’ Perspectives”with Honorable Minister Dr. Sabin Nsanzimana for which we wanted the participants to understand the role of leadership in advancing public health outcomes, discuss the challenges and opportunities for leadership during pandemics and humanitarian crises, describe the roadmap for guiding global health partnership and diplomacy efforts and explore and share resources to improve country and regional program management.
In our conversation, I described the progress of the Rwandan health system and the role leaders play in improving health outcomes for the population. I also spoke about the role of leaders in closing equity gaps while addressing major public health crises. Lastly, I highlighted on how to balance the budget allocation when deciding between adopting innovations and funding care delivery as these difficult decisions have to be made.
University of Global Health Equity- French Executive Course
October 4, 2022

UGHE holds different executive courses and amongst them is the “The Digital Health Applied Leadership Program” which aims to advance the skills and capabilities of digital health practitioners and stakeholders; initially building capacity for digital health across sub-Saharan Africa. However, to be more equitable, UGHE offers this course for Francophone Africa.
In this course, I discussed on the architecture of global health where I focused on the following points:
- The future of public health
- Global Health Initiatives
- WHO building blocks: strengthening systems and human resources for health
- Brain drain and brain circulation
- “Sustainability”
- Potential global health impact: the Rwandan experience
NIHR Global Health Research Group on promoting children’s and adolescent’s mental wellbeing in sub-Saharan Africa Launch
October 3, 2022

As co-lead of the “NIHR Global Health Research Group on promoting children’s and adolescent’s mental wellbeing in sub-Saharan Africa” study, I chaired the launch.This study is all about promoting children and adolescents’ well-being in Sub-Saharan Africa, we must recognize its timely position, as we are coming from a 3 year-period of the COVID-19 pandemic, which created the loss of millions of people but also exacerbated existing inequities such as the rise of mental health needs in developing countries. The research project will be will be delivered in two countries, Rwanda and Ethiopia from August 2022 to July 2026. It will be focused on identifying, designing, implementing, and evaluating a culturally acceptable, affordable, and cost-effective mindfulness intervention for promoting CA mental wellbeing.
Conference on Liver Disease in Africa (COLDA)
September 29, 2022

I was invited to give a talk for the Conference on Liver diseases in Africa, for which the conference was focused on empowering healthcare professionals (HCPs) to diagnose, prevent, treat, and achieve a cure for liver diseases for the benefit of patients in Africa. My talk was on ” Call for action: Key solutions” where I needed to provide solutions necessary to improve access to care, awareness and equity to fight liver diseases.
In my talk I highlighted the gaps and demands within the health sector in Africa such as the ratio of disease burden and health workforce. I also highlighted the gaps and demands within Africa needed to fight liver diseases such as the fact that the risk of death from viral hepatitis in Africa is increasing than the risk of death from HIV/AIDS, Malaria and Tuberculosis. I provided solutions in the efforts to fight and eliminate liver diseases with a focus on viral Hepatitis diseases such as focusing on testing and treatment with special focus on pregnant women which was done by Rwanda and helped achieve 90% Reduction of Hepatitis B and C new cases. Lastly, I explored the role of education to support the fight of burden of diseases in Africa using the example of University of Global Health Equity.
Seed Global: People Are the Missing Piece: Why SDG3 Won’t Succeed Without Bold Investment in Our Health Workforce
September 22, 2022

As we are facing a critical moment, there is urgency to change the status quo of what we invest in and promote the values we uphold – health, education, women for example – for inclusive growth and equity. One of the most impactful levers for change in improving health and other outcomes is also one we routinely underinvest in: our people. These have a powerful ripple effect: strengthening the response to disease burdens and improving economic outcomes.
Given this target, I was invited by Seed Global to be a panelist to discuss on” Challenging the Status Quo for our Sustainable Future: Promoting Health, Equity and Resilience”. I discussed how to turn the tide and invest in our most critical resource: people, even when it’s not the trendy investment to make for the health workforce where for instance I suggested to invest in strengthening universities in LMICs to ensure that countries can train their own healthcare workers and avoid brain drain.
As we consider the ripple effect climate change will have on the growing burden of disease, gender inequity, and growing inequities in our economy, among the pragmatic and bold solutions I suggested are to train healthcare workers in a one-health approach to identify and respond to health threats rapidly.
We also discussed on the fact that there is a movement in global development toward ‘localization’ for investment and how to remove systems of oppression in global development space.
Clinton Global Health Initiative 2022 Meeting
September 19, 2022

Alongside, Secretary Hilary Clinton and Melinda Gates, we took stage to discuss on Gender equity. In the plenary session, we discussed, about the University of Global Health Equity model of education and how it fits within the African region’s roadmap for gender equity and the broader global context. I talked about the difference between the Western Model vs the UGHE model which has a bio-social approach and teaches in a rural area and promotes gender equity. We also discussed on what transformation in gender equity looks like on the African continent and which begins by giving access to quality education to both girls and boys especially those that are vulnerable. Lastly, we touched upon brain drain in medical professions.
United Nations General Assembly-Women Leaders Network breakfast
September 19, 2022

I was invited in the series of discussion for the United Nations General Assembly. We discussed on issues around climate justice and the empowerment of the African continent, as the continent is the least contributor for carbon emissions yet it suffers the most consequences including climate change effects and others.
University of Global Health Equity- Launch of the Institute of Global Health Equity Research
September 16, 2022

The University of Global Health Equity, hosted the launch of the Institute of Global Health Equity Research. This institute is aimed at up-scaling research capacity of African researchers in clinical and medical research. The launch hosted different stakeholders including academicians from different universities, members of government institutions such as the ministry of health and other organizations Clinton Health Initiative.

“The Research Institute was created to become Africa’s leading Institute of Global Health Equity Research aimed at conducting both clinical and public health research and training the next generation of top-class researchers in Africa”
Watch full event: https://www.youtube.com/watch?v=OOvDAYLqViU
University of Global Health Equity – One Health University Network-Virtual Workshop
September 15, 2022

I was invited to deliver remarks on “Communicating Science to Inform Policy: from Research to One Health Action”. Africa One Health University Network is working to transform the training environment and approaches in universities, in a bid to develop a workforce without disciplinary barriers. Enabling students to understand and appreciate the contribution of disciplines outside their own; in predicting, detecting and responding to the kind of complex health challenges we are witnessing today.
In my remarks I mentioned that “The University of Global Health Equity is proud to be part of the AFROHUN community and as a representative of our university, we stand to address global health issues including “One health “issues such as zoonotic diseases, climate change effects and others. Because of this, we all need to take a common mission, to find solutions to address one health challenges and the way to do that is through the support of research to help generate good policies that will be effective in addressing these issues”. I also discussed why we need good policies to address One Health issues, what leaders look for from One Health advocates/scientists, what motivates a leaders to take a “policy paper” seriously, What is a turn-off to policy makers about “policy papers” (what bores them or makes them not want to read the document), and finally why is it important for One Health faculty to work with national and regional leaders to develop coherent evidence-based policies.
Partners in Health -Training the next generation of Global Health Leaders
September 13, 2022

I joined my colleagues at PIH for a discussion on how UGHE is decolonizing global health and expanding access to first-rate training opportunities. During our conversation, I mentioned that the University of Global Health Equity’s education is unique because our main focus is on global health. We are teaching our students to look beyond the diseases by teaching them about social determinants of health, humanities, history, social sciences, and among others. I also pointed out that we need to provide students with the best science, clinical skills to provide quality clinical services, but also quality knowledge on how to build the health system to exercise those clinical skills.
Draper Richards Kaplan (DRK) Foundation Retreat Panel
September 8, 2022
I was invited as a panelist by the Draper Richards Kaplan (DRK) Foundation which is a global venture philanthropy firm supporting early stage, high impact social enterprises, that believes that with early funding and rigorous support, exceptional leaders, tackling some of society’s most complex problems, can make the world a better place. This time for the retreat is for the DRK Community of social entrepreneurs, donor partners and other stakeholders to come together to listen and learn from each other and celebrate the power of our special community to make a difference in the lives of others, all the while immersed in seeing first-hand the extraordinary impact our portfolio organizations are having on our world. The purpose of the panel was to discuss challenges and opportunities in today’s healthcare, how to build more effective partnerships and implement successful health intervention in partnership with LMIC governments.
During the discussion, I highlighted on how to identify the issues in the health system and how to build it for instance using data helped to identify the problems that were in the Rwandan health system. I also explored other themes including accountability, decolonizing global health, partnerships with governments.
UGHE- Masters in Global Health Delivery Graduation Ceremony Class of 2022
August 28, 2022

On Sunday August 28, we celebrated the 44 cohort members of the UGHE Masters in Global Health Delivery program from 11 countries for completing their academic course. We were joined by distinguished guests including the First lady of the Republic of Rwanda Madame Jeanette Kagame, the Rwandan Minister of Education Dr. Valentine Uwamariya and our key note speaker Ophelia Dahl Co-founder of PIH and member of Board of Directors for UGHE who gave insightful remarks. During the ceremony, I took the opportunity to give welcoming remarks to the students.

“Since our last opportunity to gather for a commencement, we all have faced some incredibly challenging years. The pandemic has challenged us and required much innovation to overcome isolation. And in addition, our UGHE family suffered greatly along with the entire global health community when we lost one of its most visionary leaders, our chancellor and co-founder of the University of Global Health Equity, and notably a friend to all, our Muganga Mwiza, Dr. Paul Farmer. Especially, during celebratory occasions such as today, we feel this unimaginable loss. UGHE strives to carry out his legacy, and is committed to creating a preferential option for the poor through the education provided to our students for equitable healthcare services delivery.”

Watch full ceremony here:https://www.youtube.com/watch?v=nq5lZneOPAI
UGHE Masters in Global Health Delivery-Class of 2023 Orientation
August 8, 2022
At the University of Global Health Equity, we welcomed a new cohort for the Masters program in Global Health Delivery from Rwanda, Nigeria, Ethiopia, Malawi, Kenya, Liberia, Burundi, Zimbabwe, Uganda, Burkina Faso, Sierra Leone, Canada, Nepal, USA, DRC, and Syria. I delivered opening remarks to give the students insight on what to expect from being a “Lion” and being enrolled as an MGHD student. I also gave a brief overview of UGHE’s mission, values and vision.
“We believe that everyone, including the most vulnerable, deserves quality healthcare. Healthcare is a right and not a commodity.”
“This is why I am proud to let you know that you have joined a university that was recognized in the UNESCO 2022 report for our new framework that reimagines education and partnerships to address disparities.”
To learn more about this Masters program follow this link:https://ughe.org/academics/mghd/
UGHE-Global Health Summer Bootcamp Closing Session
August 4, 2022
After 9 weeks of training, the Global Health Summer Bootcamp interns concluded their course program. The participants were from Rwanda, Uganda and Jamaica. They received series of lectures from a diverse group of experts and completed desk review research on different topics addressing global health issues such as looking at the impact of COVID-19 on community health workers in Rwanda. During this closing session, interns presented their research and shared their personal experience during the bootcamp.
Harvard School of Public Health Summer Class
July 22, 2022

As a Senior Lecturer on Global Health and Social Medicine at Harvard University, I was invited by my colleague Dr. Joseph Rhatigan to give a lecture for students of Harvard’s School of Public Health. In the lecture, we discussed on the need for equity to be a core value for global health, on how the world is doing in terms of achieving this goal, and what we should be doing differently and I used the COVID pandemic example to showcase that even though there is improvement in terms of Universal Health Coverage but prior to COVID, there were already inequities which were even more exacerbated by the pandemic. We briefly discussed on decolonizing global health even though it is not a term I like to use because it exercises the old legacy of colonization in the form of white supremacy. I also discussed with the students the importance of improving health conditions for all and especially women and children because they are at the center for vulnerability when health systems are shaken or simply weak.
Global Health Summer Bootcamp – “Access to health for displaced people”
July 22, 2022

The University of Global Health Equity holds Global Health Summer Bootcamp for students in higher institutions to learn about how to deliver equitable health services delivery using the Rwandan model and other global examples. This week the topic for interns was on equitable health service delivery for refugees. I presented to the students on the Access to health for displace communities so that they can develop an understanding of health inequities of refugees and other displaced populations globally. In the presentation, I discussed about the global situation of refugees, examine the needs of displaced populations, Rwanda’s response to the refugee crisis example: political unrest and natural disaster and the UNHCR work for refugee camps in Rwanda.
Women in Global Health – High Level Political Forum on Sustainable Development Panel
July 13, 2022

I was invited by the organization Women in global health as a panelist to speak on “Women’s leadership in building back better from COVID-19 pandemic” along with other women global health leaders. I reflected on my experience as a woman leader and why men hold a higher percentage in leadership roles in health yet women are the majority of workers in the sector. I also discussed on if women should ‘lean in’ or should we be asking men to ‘lean out’ of leadership to make space for them, for which I stated that women should stand up for their inclusivity. We also discussed on change quotas in the health sector to push for more women to hold positions in global health.
Watch full discussion here: https://www.youtube.com/watch?v=NFNqrn4-Ygw
Global Health Corps Training Institute- Lecture
July 8, 2022

I was invited by the Global health Corps training institute to deliver a lecture presentation on “The Moral Obligation for Optimism in Global Health”. The fellows of this training are early career professionals, 30 years of age and below. Each of them is a national of one of our 4 placement countries: Malawi, Rwanda, Uganda and Malawi. For the 13 months of the fellowship, they assume non-traditional health roles in different placement organizations including Ministries of Health, International and grass-root NGOs with the goal to support health system strengthening. The cohort I interacted with has 52 fellows.
My presentation was focused on explaining our obligation for optimism in the fight to achieve better health outcomes and illustrate this argument with Rwanda’s health and development achievements. I talked thoroughly on health and development including benefits of optimism, the role optimism has played in improving Rwanda’s health and development and used the example of the University of Global Health Equity as the catalyst driver of health equity and development of Rwanda’s health sector.
University of Global Health Equity Graduation Address: Global Leadership in Nursing & Midwifery Executive Education Program
June 30, 2022

The University of Global Health Equity holds executive education programs that were designed to help professionals to use critical competencies that are central to health system strengthening. These customized programs help professionals in the health sector such as nurse a unique and comprehensive learning experience and with flexibility. This particular program “Global leadership in nursing and midwifery program is aimed to foster different skills that include critical thinking, problem solving, self reflection, pandemic preparedness among many others.
In my speech, I recalled that good leadership is based on equity, inclusion and collaboration. I also reminded them to always use evidence based cases to help them in decision making but also in becoming better implementers.
UNESCO Women in Science Award Ceremony
June 23, 2022

On June 23, 2022 at the UNESCO headquarters, 15 women scientists across the globe were awarded for the “Women in Science” for their ground breaking research. In the efforts of increasing women scientists recognition for their achievements and discoveries, “the Fondation L’Oréal and UNESCO for more than 20 years have worked together to help empower more women scientists to achieve scientific excellence and participate equally in solving the great challenges facing humanity“. Both institutions have awarded 100 Laureates and 5 of them have been awarded the Nobel prize.

I was awarded as the 2022 Laureate for Africa & the Arab States for my central role in expanding access to public health care for vulnerable communities in Rwanda, which was achieved through establishing, advocating for, and creating a new model of quality health care for all in Rwanda and globally.

Watch full ceremony:http://webcast.unesco.org/events/2022-06-FWIS/#
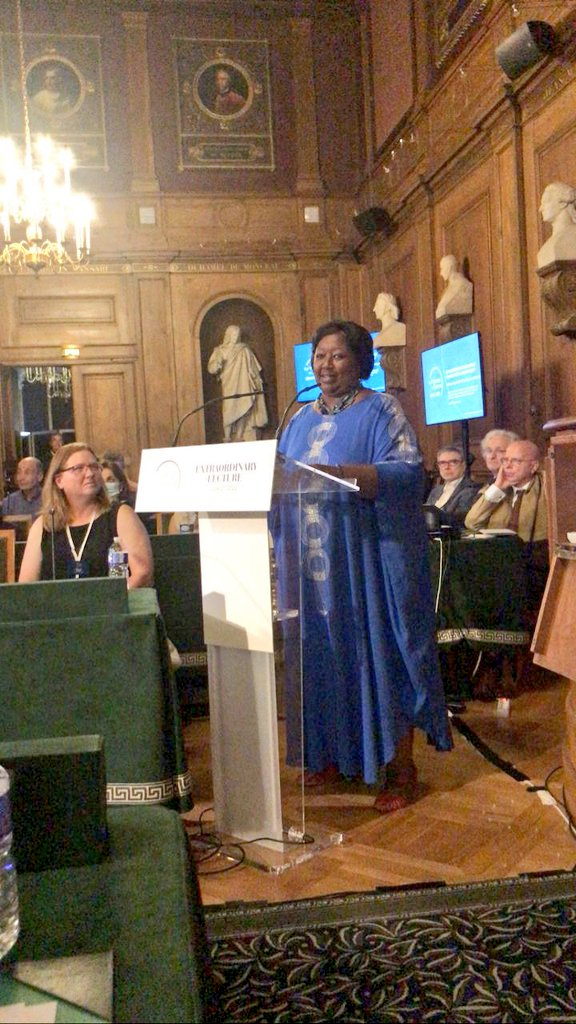
Institut de France- Academie des Sciences (UNESCO Women in Science) Extraordinary Lecture
June 21, 2022
As one of the laureates for L’Oréal-UNESCO International Awards for Women in Science, I had the honor of presenting an extraordinary lecture at the Institute of France for the French Academy of Sciences. In my lecture, I discussed the realities of the vulnerable where the poor continue to get less than what they need, as the rich enjoy more than they need. I evoked that taking an equity approach and fighting for social justice to break and these systemic barriers, is what I have worked had to do in the different capacities and positions I have lead beginning as a pediatrician and up to current as the Vice Chancellor of a quality health science education training the next generation of health professionals to deliver equitable health services, the University of Global Health Equity.
The World Organization of Family Doctors (WONCA) : World Rural Health Conference – University of Limerick, Ireland
June 17, 2022

I was invited by the University of Limerick, Ireland, to speak at the world rural health conference, which had the main theme on “Improving Health and empowering communities”. I gave a talk on ” Global Health Equity
Turning the Tide for Rural Health Outcomes”, in which I discussed factors that contribute to rural health inequities and explored strategies that can be adopted to address them. In more detail, I examined the state of inequities more generally, the movement for universal health coverage within the drive for equity and justice, explored factors that contribute to rural health inequities and provided strategies to address the contributors to rural health inequities.
Hegra Conference of Nobel Laureates & Friends 2022
June 4, 2022

I was invited for the Hegra Conference for Nobel Laureates and Friends to discuss “Retirement Security: The Cost and Opportunity of Longer Living”. People around the world live longer, which is a positive development as long as it comes with compressed morbidity. However, it means the challenges of defining retirement (age) and financing retirement urgently need to be addressed. In many countries, delaying the age of retirement is an ungrateful project that few politicians are keen to embrace. Giving the individual more agency over his or her retirement savings can be conducive to more self-financing, as long as tools that simple and accessible tools are on offer. What are the next steps to ensuring retirement security for all? How should we prepared our health systems to deal with diseases of old age such as dementia.

In the discussion, I talked about the progress on the increase in life expectancy globally, there are still inequities and challenges faced by the older populations such as the rise of NCDs and the cost of treating and supporting the elderly.
Africa CDC – Launch of the Ministerial Executive Leadership Program
June 2, 2022
I was invited by Africa Center for Diseases and Prevention, to give remarks on the role of ministers as champions of the new public health order in Africa. In my presentation, we examined the role of health ministers in relation to the SDGs, explored the health system governance, with a link to the pillars of the New Public Health Order, discussed ways in which health ministers can build and strengthen health systems and lastly provided UGHE as an example of an institution working to build capacity and support the work of health ministers.
Watch full event here:https://twitter.com/i/broadcasts/1DXxyDpQlMLJM
Harvard University- Joseph Agyepong Distinguished Lecture
May 20,2022

As a lecturer at Harvard University for the Department of Global Health and Social Medicine, I was invited to give a lecture in honor of Joseph Agyepong who is the founder and Executive Chairman of the Jospong Group of Companies, a business empire which is a conglomerate of 60 companies operating in 14 sectors of the economy. My talk was on ” Reflections on Africa’s Public Health Agenda” in which I examined the current status of public health and challenges within the health sector of Africa and provide examples of mechanisms that will drive Africa’s health agenda such as Africa’s Road to Vaccine self-sufficiency.
McGill University- Victor Dzau and Ruth Cooper Dzau distinguished lecture
May 18, 2022

I was invited by McGill University to give a distinguished lecture honoring Victor Dzau and his wife Ruth Dzau. Victor Dzau is the President of the National Academy of Medicine in the US and Ruth is the president of The Second Step, a nonprofit charitable organization that provides housing and transnational programs for domestic violence victims. My talk was about “Closing the Equity Gap in Preparation for the Next Health Threat” in which explained the root causes of inequity, how inequities were exacerbated during the COVID-19 pandemic and reflected on steps at the national and global levels to build a more
equitable future in preparation for the next health threat.
McGill University- Decolonizing Global Health Lecture
May 17, 2022
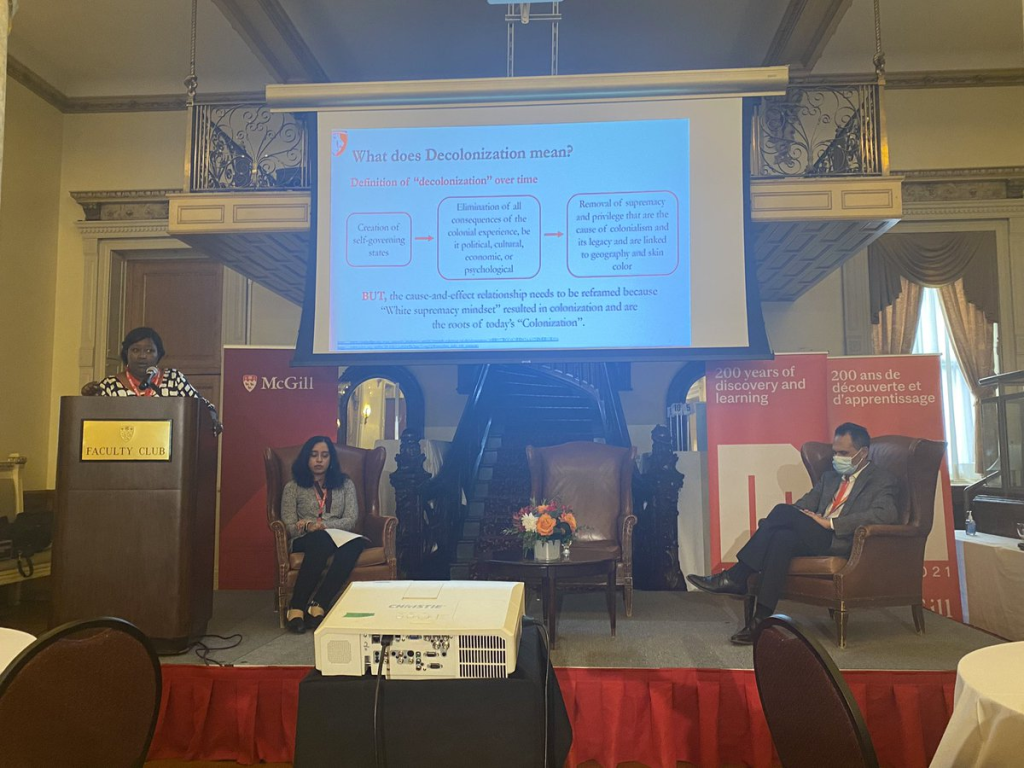
I was invited by McGill University to give a lecture on “Decolonizing Global Health”. During the talk, I explained to students what the colonial legacy looks like within global health today and explored how we can decolonize this field. I first discussed with them the meaning of decolonization; demonstrated manifestations of the western supremacy mindset to help them understand how the western supremacy mindset is cultivated. I also gave a critique of the current practice of global health and lastly, I gave the University of Global Health Equity model as an institution working to address this challenge.
University of Cape Town-Pan African Lecture
May 16,2022
I was invited by the University of Cape Town to give a lecture on the future of health in Africa. In the talk, I examined the barriers within the health sector of Africa and provide strategies to improve the population health and to ensure quality health care for the continent. More thoroughly, I explored the SDG goals related to health and the fundamental 6Ss for health, examined the gaps in service delivery and demands within the health sector in Africa and discussed strategies to provide the 6s to fight inequities. Lastly, I provide examples of existing mechanisms to ensure a healthy future for Africa, such as African Medical Supplies Platform and lastly explored the role of education in supporting the health sector using the example of UGHE.
National Institute of Health/Rwandan Health Program-Seminar on Achieving Diabetes Remission Through Lifestyle Intervention: Implications for Africa
May 11, 2022

The National Institute of Health Rwnandan Health Program was established in 2016, with the aim to help build an NIH-trained research workforce in Rwanda. The fellows are physicians who spend a year at NIH and then return home as clinician scientists to conduct research and help improve health of Rwandans. The program is led by Dr. Anne Sumner, senior investigator at the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), and Dr. Eliseo J. Pérez-Stable, NIMHD director.
I was invited to attend a seminar presented by one of the students in this program about diabetes. In my remarks I highlighted the importance of such studies because they help us in finding solutions for our communities and especially that we are seeing a rise of NCDs such as diabetes on the continent and in Rwanda.
UGHE- Executive Education Lecture with the National Health Insurance Scheme
May 9, 2022

At the University of Global Health Equity, we offer different executive courses to help develop health professionals using critical competencies central to strengthening health care delivery systems. In this course, the focus of my course lecture was on community-based health insurance in Rwanda.

In the lecture, I highlighted to the group, about the history of community based health insurance (CBHI), I talked about how it has helped to deliver equitable healthcare delivery, and achieve universal health coverage. I also briefly explored on the management CBHI through a decentralized healthcare system, the packages of CBHI according the social-economic status and discussed impact of CBHI including 91% of all Rwandans insured.
Africa CDC- Launching the second International Conference on Public Health in Africa (CPHIA 2022)
May 5, 2022

Africa Union together with Africa CDC have announced the launch of the second International Conference on Public Health in Africa, where I highlighted the following: “The 2021 Inaugural International Conference on Public Health in Africa was an extraordinary meeting that brought together renowned public health experts from across the continent, including top researchers, young scientists, clinicians, political leaders and a global audience of over 12,000 participants. Participants discussed important topics within the field of public health in Africa. This much-needed scientific platform empowered Africans to own the continent’s public health narrative, discuss COVID-19 related challenges and effective response strategies, and forge a way forward to improve population health outcomes. Most importantly, this conference highlighted the need for a New Public Health Order in Africa.”

“As we are entering a new phase of the COVID-19 pandemic, this year’s conference with the theme, Post Pandemic Recovery: Africa at a Crossroad, will build on the lessons of this crisis to further expand on the strategies needed to build resilient health systems capable of withstanding shocks while maintaining the delivery of ordinary health services. These resilient health systems will be equitable and self-sustaining to ensure that no one is left behind. The conference will once again bring experts from across the African continent to highlight the efforts in place to achieve this and the steps that we need to take collectively as a continent and independently as countries moving forward. It will continue to provide the platform for Africans to own their narrative, challenge the common perception that we cannot achieve anything on our own, and provide guidance for external partners interested in investing in our growth.”
The conference will happen in Kigali-Rwanda, from December 14 to December 16, 2022.
University of Birmingham -Forum for Global Challenges
May 3, 2022

I was invited by the University of Birmingham as a panelist to speak on advancing equitable health systems. Axis of the talk was on trust and resilience and the focus on the human dimension of health – the humans being treated, and the humans working in healthcare systems. About the human relationships of health – the quality of relationships between policies, systems and people, relationship with healthcare workers and how healthcare workers are treated. Infrastructure, buildings and capital are not the focus here. During the conversation, I highlighted the importance of building resilience especially for the vulnerable and as well the key to trust in our health systems.
UGHE-Digital Health Applied Leadership Executive Education program launch
May 3, 2022

On this day , the University of Global Health Equity (UGHE) launched the Digital Health Applied Leadership Executive Education program. UGHE as a university centered on advancing global health equity, with a focus on the vulnerable we highly value the role of digital technology in strengthening health systems, and enhancing global access to healthcare. This program is the first of its kind on our African continent and it is expected to help equip health professionals with the ability to successfully lead and execute digital health programs. For this event, I gave opening remarks where I focused how digital tools helped in the crisis of COVID-19 and how we need to leverage these solutions and capacity to innovate but also to strengthen our health sector.
UGHE- #AskProfAgnes Equity Webinar on “How to build resilient health systems to mitigate health threats due to climate change”
April 22, 2022
As a monthly continuum of the equity webinar series, I invited a panel of esteemed experts. The panelists included: Prof. Akiki Bitalabeho, Mr. Michel Jenkins, Mr. Ramon San Pascual, Dr. Tarun Weeramanthri, Dr. Corneille Ntihabose.
In the month of April, the UN celebrates World Health Day and theme for this year was: Our Planet, Our Health.

In my remarks, I highlighted: “With these many disasters, people’s displacement, and migration lead to new risks of health and well-being. During health threats such as COVID-19, the displacement of people contributes to the rapid spread of the disease and their increased vulnerability….Building health systems resilient enough to mitigate climate change and its effects will help us achieve Universal Health Coverage.”
Watch full webinar: https://www.youtube.com/watch?v=HOJs_6gO_Zc
UGHE – Research Day 2022
April 20, 2022

The University of Global Health Equity celebrated research day, an opportunity for the UGHE community to inspire and raise awareness on research done by our students and faculty, as well as the ideal time to unpack research findings on live panel presentations or to display their work on poster presentations. In my remarks, I highlighted the inequities in the research ecosystem including, partnerships, authorship amongst others.
The University of Global Health Equity Commemorates for the 1994 Genocide Against the Tutsis, Kwibuka28
April 13, 2022
In Rwanda, across the country, starting on April 7th, we commemorate for the 1994 Genocide Against the Tutsi for a 100 days.

At UGHE, we organized a Kwibuka event and we invited two guest speakers including Bishop John Rucyahana and the Mayor of Butaro that both gave really good discussions on the role of leadership and provided history lessons of what happened that it lead to the 1994 Genocide Against the Tutsis.
In my remarks I highlighted the following:
“We mourn the victims whose lives were tragically cut short during these killings and atrocities that occurred during a period of 100 days. This is why as a country every year we remember during 100 days”
“As an institution that educates for social justice and that promotes equity, we must understand how leadership matters. Extreme exclusion leads to genocide and we need to ensure that this will never happen again anywhere around the world.”
“We are united and this allows the country to progress and to now have 95% of deliveries in health facilities and the best vaccination program in the world as well as the population that has the highest trust in its health sector”
“All these improvements are due to the progress that this country has made by investing in destroying the genocide ideology, by a government & a leadership that strives to implement solutions and strategies that are based on equity and justice”
“We as UGHE, must not only continue to reinforce this mentality to fight genocide but also apply it because it is only by being equitable that we will be able to solve global health challenges”
Bocconi University Lecture
April 12, 2022

I was invited to give a lecture on “Evidenced-based, Human-centered Response to COVID-19- Lesson from Rwanda” at Bocconi University which resides in Italy. In my presentation to the students I explained the factors and strategies that contributed to Rwanda’s successful response to COVID-19, by first comparing the expectations and reality of COVID-19; evaluating the strategies that were central to Rwanda’s COVID-19 prevention and response; examining the importance of health system resilience in responding to disease outbreaks; and by exploring the role of health science education in health crisis management: the example of UGHE.
Dr. Paul Farmer’s Memorial Service at Saint-Michel Cathedral Kigali, Rwanda
April 2, 2022

On Saturday April 2nd, 2022, the University of Global Health Equity held a memorial service in remembrance of our Chancellor Dr. Paul Farmer. The ceremony was held in Kigali and attended by special guests including the first lady of the Republic of Rwanda Madame Jeanette Kagame.

All tributes of him evoked the person that Dr. Paul represented for the global health community, the world and the poor.

” Paul has left a mark in all our lives, whether it was through a one-day encounter, a lecture, many hours of working together, or 20 years of friendship like the one we shared. Paul ignited every room that he walked in, connecting instantly with people from all walks of life, no matter where they came from, who they were or what challenges they faced in life. His spirit was truly one to be treasured and cherished. Paul loved everyone he met, giving all he had with great compassion. Treating everyone with the same attention, love and respect whether it was the poorest person or the head of state. This was how he was able to move mountains, to change the world view of the poor, and to influence political leaders to make the right decisions that ultimately saved millions of lives. He had the gift to always see people in a holistic manner.”
Watch full service:https://www.youtube.com/watch?v=DdQc2phFya8
National Council for Science and Technology- 1st Rwanda Science, Technology and Innovation Conference 2022
April 1, 2022

I was invited by Rwanda’s National Council for Science and Technology as a panelist on “Strategic R&D Investment to mitigate Epidemics and pandemics”. In the panel discussion, I spoke about how we can strengthen multilateral collaboration and partnership for all stakeholders to build resilience to crises and mitigate the impact of Covid-19 and future pandemics, and talked about the existing strategies in developing countries to support and accelerate the research and innovation for the development, manufacturing, and deployment of vaccines against Covid-19 and future pandemics using the example of Rwanda.

Humanitarian Congress Vienna virtual event
April 1, 2022

I was invited by Humanitarian Congress Vienna as a panelist to discuss on Health systems and humanitarian aid: the race against COVID-19. In the discussion, I talked about on where Africa stands today in the COVID-19 situation, how health systems in Africa coped with the pandemic, what were the ripple effects of the COVID-19 pandemic in other health areas and how does a tragedy such as the Genocide in Rwanda affect the health sector.
Watch full video: https://youtu.be/WCpQWq_Qe74
CUGH Global Health Conference
March 31, 2022

I was invited by CUGH for its annual global health conference to discuss about bridging the research- implementation gap to impact population health: Examples and Priorities from Health System, Academia and Funder Perspectives.
In the discussion, I mentioned that” “We all know that implementation science research allows countries to better identify existing problems, the facilitating and challenging contextual factors as well as the strategies to address these challenges and implement the necessary actions for better population health. This implementation science approach allows countries to adapt the known strategies or EBIs successful in other countries to respond to similar problems or within the same country for emerging needs and challenges such as the COVID-19 pandemic.”
I also highlighted the importance of implementation science and how we can increase implementation science research especially for LMICs to avoid knowledge and implementation stemming from HICs.
University of Global Health Equity-Conversation avec Cynthia Fleury
March 31, 2022

Following Prof. Cynthia Fleury participation in Hamwe Festival in 2019, and as a pioneer of creating the first chair of philosophy in a hospital setting, the University of Global Health Equity is creating the first Rwandan Chair of philosophy focused on on community-based mental health.

National Council for Science and Technology- 1st Rwanda Science, Technology and Innovation Conference 2022
March 31, 2022

I was invited by Rwanda’s National Council for Science and Technology to give a keynote address on “Public Health and COVID-19 Management: Innovative Key Considerations for Developing Countries” for the 1st Rwanda Science, Technology and Innovation Conference. In my keynote address, I highlighted that the importance of innovation in management of COVID-19 pandemic in developing countries.
I discussed public health management during health crises, I provided examples of failures in COVID-19 response, I provided some key innovations for COVID-19 management in Africa, I discussed Africa’s potential to innovate and lastly I explored the role of education in increasing innovation capacity and public health management using the example of UGHE.
Watch full event here: https://www.youtube.com/watch?v=KObFIPZG1Uk
Aspen Global Innovators Group The Aspen Institute- Accelerating Breakthroughs in Global Health: The Impact and Power of Women’s Leadership
March 29, 2022

I was invited by the Aspen Global Innovators Group to discuss on “Accelerating Breakthroughs in Global Health: The Impact and Power of Women’s Leadership”. In the discussion, I spoke about my route to leadership and what were some of the gender-based challenges I faced in pursuing a research career, for which I mentioned that “I was lucky not to face too much gender based challenge in Rwanda, due to gender equity supportive policies that lead women today to have 61% of seats in Parliament – the best globally.” I also discussed on how to maintain the increased focus on the recruitment and inclusion of women in the research and policy environment, on the institutional and individual change needed and who are the exemplars in place to ensure that we continue to make progress in achieving gender equity and gender justice in global health research and policy and how to engage and bring our allies along in this world. Lastly, I gave recommendations on how to build and sustain an enabling environment for women working in global health as we reenter the world in the face of ongoing unrest and anticipated climate and economic crises around the globe such as for instance “to adapt policies that mandate equal pay for equal work with the same knowledge and experience between men and women”.
CUGH Global Health Conference- Remembrance of Dr. Paul Farmer
March 28, 2022

I was invited by the Consortium of Universities for Global Health to give a tribute for the late Dr. Paul Farmer, for the CUGH Global Health Conference on “Healthy people, healthy Planet and Social Justice”.

Here are some highlights of my remarks:
“It is an honor for me to join you to remember & pay tribute to the life of Dr. Paul Farmer, a global health visionary that the world lost too soon. It has been comforting to see the outpour of love and admiration from every corner for our dear Paul”
“Paul’s love and compassion for all who he met simply because they were human, his willingness to listen and learn and his incredible memory of everyone’s life story from the humble to the head of state, contributed to the Paul we all knew and dearly loved”
“It is an honor for me to join you to remember & pay tribute to the life of Dr. Paul Farmer, a global health visionary that the world lost too soon. It has been comforting to see the outpour of love and admiration from every corner for our dear Paul.”
ASPPH Annual meeting (Association of Schools and Programs of Public Health)-Global Vaccine Equity
March 25, 2022

I was invited by the Association of Schools and Programs of Public Health as a panelist to discuss global vaccine equity. In the panel discussion, I gave remarks stating “Currently, most low-income countries have less than 20% of their population fully vaccinated. Yet, in high income countries, most of these countries have surpassed 60% of their population full vaccination rate, such as Canada with more than 80% of the population fully vaccinated.The fact that the Omicron variant is less fatal does not mean that are we are out of the crisis. It is instead the right time to increase our efforts to get all of the world’s population vaccinated and in an equitable way especially for the world’s vulnerable.Recent research has suggested that if rich nations donated 46% of their vaccine doses, the world would be more protected against new COVID variants and there would be less deaths in low and middle income countries.”

I also talked about why these inequities in vaccine distribution are challenging, especially for many countries of Africa that have low rates of vaccination. All despite, which Rwanda has been successful with its vaccination. I also spoke on solutions to help for future pandemics such as removing debts to help countries cope with a health crisis such as the pandemic.
NIH Cancer Institute Annual Symposium on Global Cancer Research- “Rethinking Academic Global Cancer Research”
March 24, 2022
I was invited to chair a scientific panel session, for the 10th Annual Symposium on Global Cancer Research to discuss on “Rethinking Academic Global Cancer research.

The main objective of the panel was to discuss the challenges in health research and academia as well as the solutions needed to address them. In my introductory remarks, I highlighted on the need to: examine inequities in research and in global health partnerships, to reflect on the approach of Western support, looking at unethical practices in research, discussed the importance of sustainable capacity development and the need to understand the leaky pipeline in research to increase health capacity.
Watch recording: https://cugh.confex.com/cugh/2022/meetingapp.cgi/Session/1498
BMJ In-House Lecture- Decolonizing Research, Health and Academia
March 23, 2022

I was invited by the British Medical Journal to discuss how to decolonize research, health and academia. In my talk, I highlighted the need to examine the colonial legacy within global health and explored strategies to decolonize research, health, academia and peer review journal. I defined decolonization, drew parallels between current global health practices and colonialism, explored manifestation of the white mindset using the example of the global responses to COVID-19, evaluate the need to decolonize research, global health education, scientific publication and partnerships. Lastly, I presented the University of Global Health Equity as a University that is working to address these challenges.
Royal College of Surgeons in Ireland Dublin Meeting on Patient-Centered Global Surgery
March 16, 2022

I was invited by the Institute of Global Surgery at the Royal College of Surgeons in Ireland as a keynote speaker to discuss on how to avail surgical care to all in Sub-Saharan Africa . In my presentation, I mainly discussed the urgent need to ensure accessible surgical care to all across the globe, with a special focus on Sub-Saharan Africa. I also examined the fundamental issues at the center of all health equity conversations and decisions. I explained the burden of surgical diseases and the unmet need in SubSaharan Africa. I explored what true accompaniment of surgical patients looks like, evaluated the global surgery movement and examined the shortage of healthcare professionals and analyzed UGHE’s model as an institution working to address this challenge.
UGHE- MGHD Lecture-The History of Health Systems and Equity
March 14, 2022

For UGHE’s Masters of Global Health Delivery/Gender, Sexual and Reproductive Health cohort, I delivered a course lecture on the “History of Health Systems and Equity”. In this lecture, my focus was help students be able to define what a health system is, to understand the importance of the WHO health system building blocks, to learn the history of how health systems evolved beginning with primary health care movements, to understand equity in health systems and the importance of health sciences education.
UGHE- #AskProfAgnes Equity Webinar on “Improving challenges of women and girls in Science using Lessons learned from COVID-19”
March 8, 2022
As a monthly continuum of the equity webinar series, I invited a panel of esteemed activists for women in science. The panelists included: Tsion Yohannes, Dr. Renzo R. Guinto, Prof. Flavia Senkubuge and Prof. Marleen Temmerman.
In the month of February, the International Day of Women and Girls in Science is celebrated and in March, the International Women’s day is also celebrate. For this month’s equity webinar series, the panelists discussed on the challenges faced by women and girls in science in Africa, the challenges women in Asia have faced, the global perspective of these challenges and how we can improve and overcome these challenges.

In my remarks, I recalled on “paying tribute to a giant leader who shaped the future of global health” the beloved Dr. Paul Farmer, who has “left a legacy that will impact far beyond global health” for which “the best way to honor his memory will be for all of us to stand stronger together doing what he loved most: which is fighting poverty and disease, promoting human dignity with a focus on the most vulnerable, and promoting equity”.
In relevance to the topic, I mentioned some key facts: “According to UNESCO’s forthcoming Science Report, only 33% of researchers are women, even though they represent 45% and 55% of students at the bachelor’s and master’s levels of study respectively, and 44 % of those enrolled in PhD programs. Specifically in the health sector, 70 % of health and social care workers are women, and yet they are paid 11% less than their male counterparts.” These facts were even more exacerbated by the pandemic. However, the promise is that “Studies have proven that when women are integrated in research teams the collective production of the team improves”, therefore women should participate and included more in research.
Watch full webinar: https://www.youtube.com/watch?v=sgUq8zDpHX8
UNESCO & Ministry of Education of Rwanda-Fourth African Regional Sciences, Technology and Innovation Forum
March 2, 2022

I was invited by the Ministry of Education in Rwanda, to take part in the “Fourth African Regional Sciences, Technology and Innovation Forum” as a panelist on “Science Technology Innovation and Gender”. In my remarks, I highlighted the importance of implementing innovation in education, especially with threats such as climate change and pandemics rising up. I also mentioned the need to improve our human resources especially in the health workforce and the critical need to bridge gender gaps especially in STEM fields where the need for women to be acknowledged for their work and to be trained with technology to benefit their communities is crucial.
UNU-IIGH dialogue: Shifting power in global health Decolonizing Discourses
March 1, 2022

I was invited as a panelist by the United Nations University International Institute for Global Health for a discussion on South-South partnerships and their own power dynamics. In my remarks I stated that there is evidence of inequitable partnerships within global health in all aspects including academic, research, or program implementation settings. The way to change this pattern of inequity is first “to acknowledge the knowledge and expertise that exists within the global South”, secondly “to ensure that local experts in global South determine the topic of research and the choice of program implementation when it is being done in their own countries”, third “partnerships between global North and global South institutions needs to focus on building and strengthening the capacity of those in the latter” and lastly “the global South needs to leverage the knowledge that exists within our countries”.
ECOWAS- Universal Health Care Summit
February 25, 2022

I was invited by the West African Health Organisation (WAHO) for the high-level ECOWAS (Economic Community of West African States) Universal Health Coverage Summit as a key note speaker. During my presentation, I discussed the importance of Universal Health Coverage (UHC) in improving the population health and the strategies required to achieve it. I highlighted on defining on what UHC means, the importance of UHC and I also explored the different strategies for achieving it listing the six “S” that include : Staff, Stuff, Space, Systems, Support and Sustainability. Lastly, I examined the contribution of the education sector to the achievement of UHC, with UGHE as an example of a health science institution driving forward the UHC agenda.
Connected Women Leaders -Women’s Empowerment Learning Journey
February 20,2022

As a member of the connected women leaders, on this occasion, I was invited to give a motivation speech iterating my journey as a woman in science. In my speech, I highlighted that I have always had a need to improve the conditions of other fellow women scientists and to change the status quo. I talked about how I came back as a pediatrician after the 1994 genocide and was seeing children die from preventable diseases, which pushed me to learn and acquire knowledge about things that I didn’t have in the first place such as ordering incubators with precise details. I then talked about my shift from clinician to public health and how I co-founded the University of Global Health Equity.
UGHE-Opening Session Musical Archive Exhibition Workshop
February 16, 2022

The University of Global Health Equity with the Rwanda Heritage and Cultural Academy organized a musical archive workshop that will kick-off planning the exhibition that will discuss the role of music in Rwandan society as well as links between music, heritage and mental health for which I gave introductory remarks highlighting how UGHE has played a role in incubating a series of archives for art in global health such as the annual Hamwe Festival that celebrates art and health.
UGHE launch of Center for Equity in Global Surgery
February 8, 2022

The University of Global Health Equity is home to different centers that aim to strengthen global health equity in different domains that require solutions for major problems affecting vulnerable populations. For instance we have a Center for Nursing and Midwifery with the aim to maximize the contribution of the nursing workforce and their roles within inter-professional health teams. Now, UGHE has launched the Center for Equity in Global Surgery with aim to shift the center of gravity of the global surgery movement from HICs to LMICs, and no less to rural areas where the vulnerable have the least access to surgical care.
In my remarks, I noted on the following:
“Many have said it already and we have experienced it long enough, that the vulnerable are denied access to quality healthcare. This inequity is especially evident in surgical care for the vulnerable living in rural areas who have no or very limited access to quality, safe, and holistic surgical, obstetric, and anesthesia care. Too often, surgery has been portrayed as a luxury in LMICs with more emphasis on a set of primary healthcare services rather than on providing specialized care such as surgical care. This is why global health in the last few decades has focused on providing funds for infectious diseases instead of the holistic care needed by the people living in LICs, especially in rural areas. This has no epidemiological ground. For instance, 40% of global health funding is allocated to infectious diseases compared to the mere 1.8% that is provided for NCDs, a majority of which require surgical interventions. Furthermore, the poorest part of the world receives only 3.4% of the 234 million operations performed annually, yet they consist of 34.8% of the global population.”
“The global surgery movement – the equivalent of global health within the field of surgery – was created to redress the inequities created by this low value attributed to the lives of those in LMICs. But this fire in the global surgery movement was accompanied by surgical missions led by foreign surgeons who aimed at promoting their social standing through photo opportunities with patients and local surgeons rather than collaborating on knowledge sharing.”
To watch full ceremony: https://www.youtube.com/watch?v=2vnH095d5C4
UNICEF- Partnerships in Implementation Research
January 31, 2022

I was invited along with other panelists, collaborators and partners of UNICEF to give an overview of how should Implementation research be applied. In my speech, my key message was that “There is a need to expand its use and to leverage existing and new partnerships to strengthen implementation science research capacity within national governments, implementing partners, local and international academic institutions, and UN agencies such as UNICEF.Training in implementation science should be imbedded within all pre-service education and provided to health professionals in service.For instance, supporting women’s education and empowerment within the financial and employment sectors can improve children’s and women’s survival”.
UGHE- Medical students (MBBS) Lecture on “Bending the Arc” documentary
January 27, 2022

I was asked to participate in a Q/A session for UGHE medical session on “Bending the Arc” documentary film that Paul Farmer and I participated in and contributed to. The film is set to speak on global health challenges including MDR-Tuberculosis and HIV-AIDS response in Haiti, Peru and Rwanda. The story depicts how the founders of Partners in Health for which Paul Farmer was a part of struggled to convince world leaders to give life saving treatment to poor resource settings, even with scientific evidence this could be done. For those interested to watch the full documentary, it is currently streamlined on Netflix.
Prince Mahidol Award Conference (PMAC)
January 27, 2022

I was invited for the Prince Mahidol Award Conference, to participate in a panel that discussed on “What Extent Will the COVID Pandemic Affect Achievement of the SDG Goals”. The Prince Mahidol conference is an annual international conference focusing on policy-related public health issues of global significance with a mission to bring together leading public health leaders and stakeholders from around the world to discuss high priority global health issues, summarize findings and propose concrete solutions and recommendations.

During the discussion, I spoke about what impact did the COVID-19 Pandemic have on the chances of African countries meeting the SDGs. I also spoke on SDGs achievement and successes in Rwanda, and gave examples on gender equality such as female representation in the parliament which is the highest in the world.
Duke University-The Victor J. Dzau Distinguished Lecture in Global Health
January 26, 2022

I was invited by Duke University to talk about restoring global solidarity for the road to pandemic recovery.
During the conversation, Paul Farmer and I spoke about how we first met in the global health arena and how we wanted to make great changes and create impact that would change the world such as creating the University of Global Health Equity which is a medical and health science university in rural Rwanda and was built to give opportunities for young people and to help serve the vulnerable globally.
Watch more on our conversation: https://www.youtube.com/watch?v=OLeXX3kjbzM
University of Global Health Equity-Book Talk with Author of “Fevers, Feuds, and Diamonds: Ebola and the Ravages of History”: Dr. Paul Farmer
January 25, 2022

As a colleague and co-founder of the University of Global Health Equity, I was asked to present my long-term friend Dr. Paul Farmer for his latest book titled “Fevers, Feuds, and Diamonds: Ebola and the Ravages of History”. The book is a deep dive into the history of West Africa and how it all ties together with the poor response of the Ebola outbreak that occurred in West Africa. For example, Africans were not allowed to study Medicine or Geology, yet colonizers had built hospitals, which depicts why there is limitation of the 4 S’s (Staff, Stuff, Space, and Systems). He also describes his personal experiences with Ebola patients, which are daunting images. Lastly, he criticizes the fact that the western way of dealing with epidemics is to always control the disease which was not the correct way to respond to Ebola, patients remarkably needed intensive and supportive care.
Dartmouth University-Global Health Systems Lecture Case Discussion HIV in Rwanda
January 20, 2022
As a Professor at the Dartmouth College, I was cordially invited to speak to students in Global Health Systems Delivery on the case of HIV in Rwanda. In my discussion with the students, I spoke on how the HIV program began in Rwanda, I spoke on the how Rwanda has been able to achieve a higher HIV universal coverage than in other countries. I also highlighted the influence of the HIV program in improving other health outcomes such as maternal survival.
Africa HealthCare Foundation-2nd Europe Africa Health Summit
January 19, 2022

I was invited as to give a keynote address on health workforce development to create resilient health systems by the Africa Healthcare Foundation. In my discussion, I emphasized that health is at the center of human development and that Africa is experienced at providing community health services. I mentioned that the quality of healthcare education and specialized is still a challenge in Africa and in addition brain drain of those that are specialized. Therefore, “we need to fight brain drain by building legal frameworks and train doctors in management and advocacy because they know the real issues”.

Watch full video here:https://youtu.be/MmOmXob6uXY
Africa Europe Foundation-Sideline event for the 1st Conference on Public Health in Africa
December 17, 2021

In continuation of the discussion for the Conference on Public Health in Africa and as a member of the Africa Europe Strategy Group on Health, I was asked to participate on a panel discussion on “Challenges in a Changing Health Landscape”. In the discussion, I highlighted on the role of international partners in supporting the ambitious goal for greater autonomy in the manufacturing and production of medical supplies in Africa. I also spoke on how to find a balance between today’s urgencies and the need to prepare for a future health workforce that will operate differently and needs different skills.
Rwanda Pediatric Association- 5th Annual Scientific Conference
December 16, 2021

On the last day of the conference, I was asked to be the keynote speaker for closing ceremony of the conference. In my speech, I presented on the role of pediatric associations in solving child health related issues but also improving standards of pediatricians around the world. I highlighted that as pediatric associations, we have to be advocates for children, share our best practices, increase capacity building in pediatric research, improve our management capacity, use innovation and technology, find ways to retain pediatricians, find ways to build professional and social satisfaction, improve private pediatric care and lastly to improve training of the pediatricians.
Africa CDC & African Union-Developing, Producing and Delivering Oral Therapeutics for COVID-19- Special session for the 1st Conference on Public Health in Africa
December 15, 2021

In continuation of the 1st Conference on Public Health in Africa, I moderated the panel on Developing, Producing and Delivering Oral Therapeutics for COVID-19. The discussants were:
- Dr. John Nkengasong, Director, Africa CDC
- Dr. Trevor Mundel, President of Global Health, Bill & Melinda Gates Foundation
- Dr. Julie Gerberding, Executive Vice-President and Chief Patient Officer, Merck
- Dr. Salim S. Abdool Karim, Director, CAPRISA
To watch full session: https://www.youtube.com/watch?v=-Xm0xvcVlCM
Rwanda Pediatric Association- 5th Annual Scientific Conference
December 15, 2021

As co-founder of the Rwanda Pediatric Association, I had the pleasure to participate in their annual scientific conference. In the first session, I presented on a research work done on ” Maintaining Health System Delivery of Evidence-Based Interventions for the Reduction of Under-5 Mortality during the Period of COVID-19 in Rwanda”. In my presentation, I spoke on the global disruption of essential health services including maternal, newborn, child and adolescent health and nutrition services. Our goal was to understand if and how health system-delivered EBIs (Evidence Based Interventions) targeting amenable U5M (Under 5 mortality) were maintained and what strategies were used to identify, prevent, or respond to EBI drops; factors that helped or hindered the response to COVID-19-related threats to EBI uptake and delivery; and the previous efforts to implement these EBIs between 2000-2015 supported the work to maintain EBIs during the pandemic.
Africa CDC & African Union-Inaugural 1st Conference on Public Health in Africa
December 14, 2021

On December 14 of the year 2021 we inaugurated the first conference on public health in Africa with the leadership and organization of Africa CDC and African Union.
Although, we would have preferred to have it physically held, we held it virtually with organized abstract presentations from our African scientists, panel discussions, debates and video content to showcase the responses of the pandemic in Africa.
In my Inaugural session speech I highlighted on the fact that Africa has responded relatively better to the pandemic than other continents and that we observed that African countries cannot rely on the western world for their domestic health needs. I also mentioned that “My wish is that this conference will provide the much-needed platform to discuss the components of this New Public Health Order and identify strategies that will ensure a safer and healthier future for our continent.”
Watch full session here: https://www.youtube.com/watch?v=UyJCXCKPY-w
Africa CDC & African Union-African Women Leaders in Public Health through History-Sideline event for the 1st Conference on Public Health in Africa
December 13, 2021
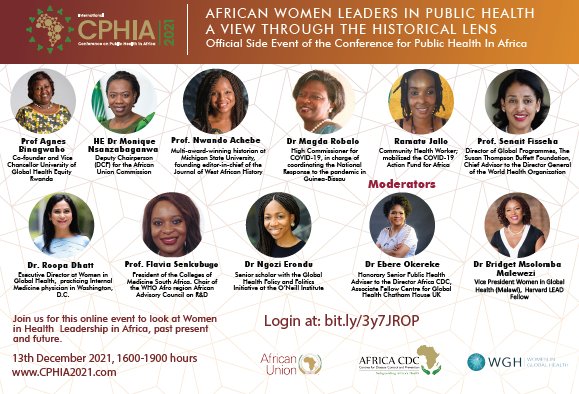
As co-chair of the first conference in public health in Africa, I was delighted to take part not only in the conference but other events and important debates that complemented the historical moment of this conference on our continent. The event was organized by Africa CDC and global health in women in Global Health. In my discussion, I mentioned that women are the true drivers for health improvement and therefore we should create enabling environments, make gender equity central in recruitment & training, support them in their careers and places of work.
UGHE & PIH-Butaro Hospital Expansion Ceremony
December 10, 2021

The Butaro District Hospital which is located nearby our campus at UGHE and where our medical students perform their clinical rotations plans to build a new ward expansion. This expansion is significant for both UGHE and the community of Butaro because they will have access to many more health care services and our students will have more services to learn from.
Forum Galien Afrique
December 10, 2021

I was invited for another panel participation for the Forum Galien Afrique to discuss on One Health-One Africa: A New Agenda on Governance and Post-Covid Economic Growth in Africa. In the discussion, I spoke on the strategies Rwanda has used to help rebuild the health system after the genocide and how they also have helped for COVID-19 response. I also spoke on how the University of Global Health Equity is helping to train the next generation of health professionals on the continent.
UGHE-White Coat Ceremony
December 9, 2021




At the University of Global Health Equity, we celebrated the first white coat ceremony for our Medical students, Class of 2025. With the pandemic many of the events have been organized virtually and we have followed the national regulations. Therefore, we were not able to celebrate our students milestones in normal circumstances as we usually do. It was both an honor and a pleasure to see this cohort move to the first step of choosing a medical professional life.
Watch ceremony: https://www.youtube.com/watch?v=NQI2_ppu-mg
Forum Galien Afrique- 4th edition
December 8, 2021

I was invited by “Forum Galien Afrique” which celebrates pharmaceutical innovation and medical research to take part of a conversation on reform for health training. In my participation, I shared a video of the University of Global Health Equity and explained how we are changing the face of health science education and training and how we are creating solutions to address health workforce issues in Africa.
Watch UGHE video:https://www.youtube.com/watch?time_continue=2&v=GjEsq-Q6hnI
UNU-IIGH -Gender Equality and Health in Africa Panel
December 8, 2021
I was invited as a panelist by the United Nations University International Institute for Global Health to speak on the topic: Gender Equality and Health in Africa: a collaborative platform to identify research priorities and best practices in the wake of COVID-19″. In my discussion, I highlighted that we need to be more connected within systems and structures and to be pro-active in creating a stronger network for women. I also mentioned that we need to approach young adolescents girls for the network we want to create for them. Lastly, I mentioned that we need to give more fuel and action for to tackle issues faced by women, for example by reporting more on GBV cases.
Watch Full video here:https://www.youtube.com/watch?v=PzFLgQlh5UM
ICASA (International Conference on AIDS and Sexually Transmitted Infections in Africa) Satellite Session
December 7, 2021

I was invited to speak on a satellite session organized by ICASA (International Conference on AIDS and Sexually Transmitted Infections in Africa) to discuss on if Global Health Initiatives that focus on HIV contribute to building stronger, more resilient health systems. In my response, I evoked that vertical programs that focus on a specific disease are not what build stronger health systems but how governments choose to use the money for fighting the disease in strengthening their health systems. This is the case of Rwanda, that has achieved many of its milestones in health system building using funds for AIDS.
University of Maryland Baltimore-A vision of Global Learning for Health Equity
December 1,2021

I was invited by the University of Maryland Baltimore to participate in a panel discussion to discuss the vision of global learning for health equity. In the talk, I discussed on the way to advance global learning which by challenging the white supremacy mindset and to have partnerships that are equal and with mutual respect.
“We need to challenge the white supremacy mindset that always considers white people to be superior to those with other skin colors. They are various approaches that we can adopt to challenge this sentiment that is deeply rooted in the culture of Europe and the US. This mindset, whether conscious or unconscious, must be actively challenged in order to create the opportunity for respectful, dignified and cross-learning. It will also allow us to challenge the North-South paradigm that assumes that knowledge always flows from the North to the South – never the other way around. We need to build fair partnerships in global health that are truly based on values of mutual respect and mutual benefit. For instance, LMIC partners need to have an equal say in the design and implementation of research projects or in service delivery.”
UNESCO Women in Science Awards -Young Talent Program
November 24, 2021

I was invited along with a fellow Laureate Prof. Catherine Ngila to share my experience with young women scientists. I shared my story by highlighting that the women in Rwanda have been my source of inspiration even in moments of uncertainty. I also commended UNESCO for promoting young women scientists and I also mentioned that what was achieved because of the gender equity agenda in Rwanda should be applied in research to obtain similar results.
Consultative Workshop on Health Workforce Development Health Workforce Measurement and Metrics
November 23, 2021
I had the honor to host a session on health workforce measurement and metrics. In my remarks I highlighted that health is the pillar of human and economic development, so we should push for the improvement of our health systems in this context.”Health resiliency must be strengthened at all levels of the healthcare system from the primary to the tertiary levels. For the community health system, Africa can support this effort in solidarity with no need of external assistance because we have the capacity and expertise on our continent. We can learn from experiences from countries like Rwanda and Ethiopia that have developed very successful community healthcare worker programs that have expanded the reach of the healthcare system into the communities”
UGHE-#AskProfAgnes Equity Webinar on Improving Road Safety using Lessons learned from COVID-19
November 23, 2021

As a monthly continuum of the equity webinar series, I invited a panel of leaders to discuss how to improve road safety using lessons learned from COVID-19. The panelists included: David Ward, Irene Bagahirwa, Iain Cameron and Jessica Truong.
In the month of November, the World Day of Remembrance for Road Traffic Victims (WDR) is commemorated each year by the United Nations to remember and pay respect to the many millions who lose their lives or are injured on the world’s roads. In this month’s equity webinar series, the panelists discussed on the Commonwealth Road Safety Initiative; on the situation in Australia in terms of challenges faced during COVID-19 and lessons learnt to reduce road traffic fatalities; on the Situation in Africa (Rwanda), challenges faced, and lessons learned to successfully reduce road traffic deaths and injuries; and on the Global Plan for the Decade of Action for Road Safety and what we can do to achieve it.
In my remarks, I recalled on the need to improve roads, develop policies, laws and strategies to increase road safety because during the pandemic people still increased speed with low traffic movement.

Watch Full video here:https://www.youtube.com/watch?v=kJP2dogoJxY
Atlantic Fellows Virtual Convening
November 10, 2021
I was invited by the Atlantic Health Fellowship program to lead a seminar concerning leadership. I shared my experience and work as the Minister of Health of Rwanda and the COVID-19 response in Rwanda and globally. In my presentation I discussed Rwanda’s history after the 1994 Genocide Against the Tutsis; I examined Rwanda’s equity agenda and its positive results;I explored the need for and the mechanisms to build accountable leadership; I described the role of a visionary leadership led by implementation science; I also explored leadership successes and challenges during COVID-19 and lastly I presented Rwanda’s COVID-19 response as an example.
UGHE-Hamwe Festival 2021
November 10, 2021

The University of Global Health Equity organizes annually the Hamwe Festival which is an art festival that links creative industries and the health sector. This year’s theme of the festival will explore the social changes since COVID-19.

At the opening, I had the honor of taking part of a panel discussion with Dr. Sheila Davis (CEO of Partners in Health) and Christopher Bailey ( Arts and Health leads at World Health Organization) to discuss the role of arts in health. In the discussion, I highlighted that this Festival is a unique platform and each year is an opportunity for us to create a linkage between health professionals and artists. I talked about the way people were affected by COVID-19 and how arts can help during these rough times because art has been used previously in helping with mental health, in improving performances. I also highlighted the need to do research and translate this research into policies and strategies to see how art can be integrated in the healthcare system. We also received the Honorable Minister of State for Youth and Culture Edouard Bamporiki who gave his remarks as well on how arts are getting integrated into the education system.

Watch Full video here: https://youtu.be/iQY6EPQgIWQ?list=PLKf7qRq4AS5fugQ6E4zpN1pWkvbi8SdNK
UNESCO World Science Day for Peace and Development
November 5, 2021

UNESCO -Poster
I was invited as a laureate of the 2022 L’Oréal-UNESCO For Women in Science Awards by UNESCO to celebrate the world science day for Peace and development. Along with other Laureates, we discussed on the theme of “Global Health in a Changing Environment- Building climate-ready “. In the discussion, on my vision of a global health equity taking the experience of Rwanda health care system. I also highlighted, the need to make a link between health and the environment because it both affects the vulnerable.
Nigeria Health Watch-The Future of Global Health Conference
November 4, 2021

I was invited by the Nigerian Health Watch to discuss on elevating the importance of gender equality in achieving quality of Women’s Health. In the discussion, I stated that we need to focus on general quality care for both men and women, secondly we should continue to develop digital health access by increasing private public partnerships and the private sector should be involved in manufacturing and support health facilities. I also spoke about what UGHE is doing to keep a gender equity agenda, which includes our admission policies for 70% in medical school and 50% for in Master of Global Health delivery as women because we feel the need to increase the number of women that are global health leaders and the number global researchers.
USGLC Global Impact Project – 2021 Annual Virtual Reception
November 4, 2021
I was invited by the U.S. Global Leadership Coalition (USGLC) to give deliver a special toast, particularly recognizing the importance of the private sector response to expanding access to health for Rwandans living in rural areas. USGLC is a nonprofit organization formed by a coalition of American businesses and NGOs, senior national security and foreign policy experts, faith-based and community leaders from across the United States who promote increased support for the United States’ diplomatic and development efforts among both politicians and the public.
“Our health sector is based on the results of private sector that contributed to increase the health of our population through vaccines that save children’s lives, to expanding access to health for those in remote areas with digital health, to supporting the response to emergency health threats such as COVID-19, and to research projects that provide critical insights for the improvement of healthcare delivery. Going back in time I especially commend the U.S. Global Leadership Coalition’s support for the fight against HIV that saved so many in the developed world.”
UNU-What’s next for Global Health? Views from the Global South
November 3, 2021
I was invited by United Nations University – World Institute for Development Economics Research to be a panel speaker to discuss the future of Global Health. In the discussion, I talked about the major lessons drawn from COVID-19 crisis about global health governance, where I highlighted that health is at the center of all development, that COVID-19 exacerbated inequities, there was a lack of respect to ethics especially from rich countries. I also mentioned that regional organizations should collaborate for the future of health governance to help respond and prepare for such a health crisis; they should collect and share important research on health data and help strengthen the production of life-saving tools such as vaccines.
Global Philanthropy Forum 2021
October 21,2021

I was invited by the Global Philanthropy forum to speak about the global movement towards health equity as a panelist. The Global Philanthropy Forum is a peer-learning network of philanthropists and social investors committed to advancing international causes. During our discussion, I mentioned the fact that “Health Equity means that we share with everyone what is available according to what is the needed of each and everyone and for them to advance in their journey and in order for them to reach their full potential and to be able to achieve better health outcomes. If we are speaking in global terms, it is simply put at a bigger scale, but the principle is the same that we apply because the goal is to make sure everyone is served with equity not equality meaning those with less receive the most.” I gave examples of this definition such as increasing immunization rates for children to prevent them to getting infected from preventable diseases. I also spoke about the strategies used in Rwanda to build an equitable health system which includes trust, accountability, solidarity and cultural humility.
Watch highlights: https://www.youtube.com/watch?v=hrHFT8rZBNw
Africa Health Congress-Future-proofing healthcare post-pandemic – what does sustainability in Africa look like
October 18, 2021
I was invited by the Africa Health Congress to be a panelist and speak about opportunities on how to build the health digitalization capacity of Africa. In my talk I mentioned that Africa has the potential to build this capacity because “80% of Africa’s population has a mobile phone subscription, today, at least 1/4 of the African population has internet access and by 2030, the continent could increase this internet penetration by 3/4 of Africans projected to become internet users. Lastly mobile technologies alone have already generated 1.7 million jobs and contribute $144 billion to the continent’s economy, or roughly 8.5% of GDP.” In my talk, I also mentioned that to stem brain drain in Africa we need to “create a legal framework like in football that doesn’t allow you to steal talent, allowing people to be compensated for their job and to educate more people”.
CUGH Virtual Summit- The Road to COP27
October 15, 2021

As a member of the Consortium of Universities for Global Health (CUGH), I was invited to give opening remarks for the virtual summit which was to address climate change and how to improve health outcomes.
I highlighted the following:
“Africa produces 16 times less CO2 emissions than the US, while Africa produces less CO2 emissions it remains the primary victim of climate change”
“Between 1970 and 2019, Africa recorded more than 1600 disasters and lost more than 730,000 lives, five times more lives lost than Europe for the same amount of disasters within the same period”
“Solutions to reducing CO2 emissions are full hypocrisy, if Africa produces little CO2 emissions and western countries are penalizing Africa for using fossil fuels while they do not apply these rules themselves”
Watch full video here:https://www.youtube.com/watch?v=lN4t9T9toug
Bill and Melinda Gates Foundation-Prepare to Respond Forum
October 12, 2021
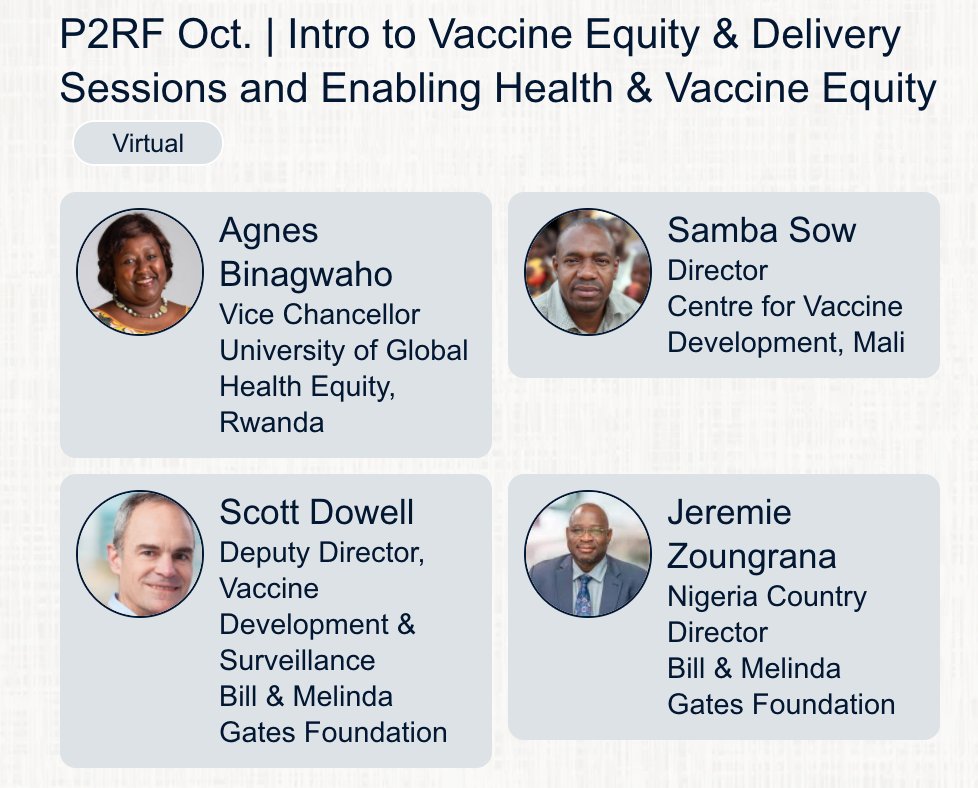
I was invited by the Bill and Melinda Gates Foundation to be a panel speaker along with Prof. Samba Sow. In the panel, I discussed on how future health professionals should be trained where I mentioned they should grow cultural humility, practice compassionate care and use implementation science. I also talked about what are the hopeful programs that show that vaccines on the African continent will be scaled up where I mentioned that we have partnerships that have begun for vaccine manufacturing including Rwanda and Senegal, existing manufacturers such as South Africa. We also discussed on using traditional medicine in Africa and I mentioned the colonizers destroyed this heritage, yet it is widely used in Africa as the primary source of health care.

T20 Summit “Vaccines and Health Care: Global Public Goods”
October 5, 2021

I was invited by T20 Italy to discuss vaccine roll-out campaign and access to vaccine for Africa. In my talk, I highlighted that rich countries have hoarded doses and now the issue is that there are no available vaccines on the market. I also noted that Pfizer keeps increasing their prices which makes it difficult for developing countries to purchase them. Lastly, I mentioned what needs to be done to increase capacity for global vaccine manufacturing , which is to increase human resource capacity, develop necessary infrastructure, waive trips waiver and to attract financial investment.

Watch full session: https://www.youtube.com/watch?v=NNYwjzefNJ8
UNDWF-Data Driven Vaccination Strategy for a COVID-19 free world
October 5, 2021

I was invited by the United Nations World Data Forum to be a panel speaker to discuss the different ways data was used for vaccinations strategies in different countries including Rwanda, Bangladesh, USA and Argentina. In the discussion, I highlighted that Rwanda performed an assessment of logistical needs, cold chain capacity equipments, a priority list needed to implement a well-coordinated vaccination strategy.
Baylor University-2nd Baylor Global Health Week
October 4,2021
I was invited by Baylor University to give a lecture on how to build equitable partnerships. In my lecture, I discussed needed changes in partnerships to improve health equity. I spoke on mission and values we share between UGHE and Baylor University. I provided an overview on the challenges in current partnerships, challenges faced due to the shortage of health workforce in Africa, the Effects of COVID-19 pandemic on health education, types of equal partnerships, the roles of universities in achieving the SDGs and gave recommendations for successful partnerships.
Boston College-The Rising Global Cancer Pandemic Conference
October 2, 2021

I was invited by Boston college to present on prevention and treatment for cancer in Africa. I spoke on the interventions and actions needed to fight the rise of cancer in Africa, in the context of social justice and by giving the example of Rwanda.
In my presentation, I discussed the Global and regional status of non-communicable diseases, I compared cancer threats in Africa versus high-income countries with the example of the USA, I highlighted contributing factors leading to inequalities in cancer care with a comparison of Africa versus USA. I also demonstrated some of the African innovations and strategies to fight cancer in Africa including the example of Rwanda for the HPV vaccine.
European Health Forum Gastein-Strengthening health systems worldwide – what next for the global health approach?
October 1, 2021

I was invited to be a panel speaker by the European Health Forum Gastein to discuss on how to strengthen health systems worldwide. In my discussion, I spoke on the impact of partnerships between Africa and EU has had on health systems in Africa. I highlighted that our history of colonialism has had impact on health in Africa in a negative way, however that our relations have evolved. Despite the evolution in relations, Africa is still treated as a recipient of donations instead of an equal partner. If we want to see change, Africa should be an equal partner and partnerships should focus on equity, mutual respect and improving social determinants of health.
Stanford University (Global Health Equity Course)
September 29, 2021

I was invited by Stanford University to give a lecture on global health inequities with a focus on COVID-19 and gender equity. I first gave the students a brief overview of my background, I talked about some of the challenges I faced in my career as a woman, as someone who did not speak the local language and how my inspiration to fight for social justice stems from looking over survivor women of the genocide. I talked to them about some of the successful programs that have helped achieve equity in Rwanda such as the gender-based violence prevention programs which offers integrated medical care, psychosocial support, legal support for victims of domestic violence . I told them about challenges that women in the global South face such as making their voices and ideas considered in the global arena.
Further along, I gave examples of the heath inequities between women in the North and the global south such as the disparities in cervical cancer where the US has sufficient funding to support free cancer treatment for women, yet LMICs financial support is limited.
I also talked about the effects of COVID-19 on women in Rwanda which is reduction of salary and employment challenges and working longer hours. I spoke on why UGHE is making a difference to change this, which is to carry on the equity agenda including one for gender where we have 70% of women enrolled for medical school and 50% for the master in global health delivery as female.
Lastly, I spoke on how social determinants of health in Rwanda have improved but that we still need progress.
Bill and Melinda Gates Foundation-Goalkeepers 2021
September 29, 2021

I was invited for Bill and Melinda Gates Foundation 2021 Africa celebratory event where I was asked to discuss briefly on what my university is doing to advance in health education and fight for equity. The goalkeepers are a community of change makers who are advancing the global goals in diverse ways. These leaders represent a range of cultures, profession and interests.
European Health Forum Gastein- Inclusive Multilateralism
September 27, 2021

I was invited by the European Health Forum Gastein to take part of a panel debate on multilateralism along with Sandra Gallina (Director General, Directorate-General for Health and Food Safety and Hans Kluge ( Regional Director, WHO Regional Office for Europe).
In my discussion, I talked about the fact that Europe does not represent as a fair partner because of their actions during the COVID-19 response. I recalled on European leaders that they need to have more accountability and if we want multilateralism it needs a change where there is fair partnership and one that saves more people.

Watch Full video here: https://www.youtube.com/watch?v=hhXQ7AE_YFo
UGHE-#AskProfAgnes Equity Webinar on South-South Cooperation in education to Strengthen Development
September 24, 2021
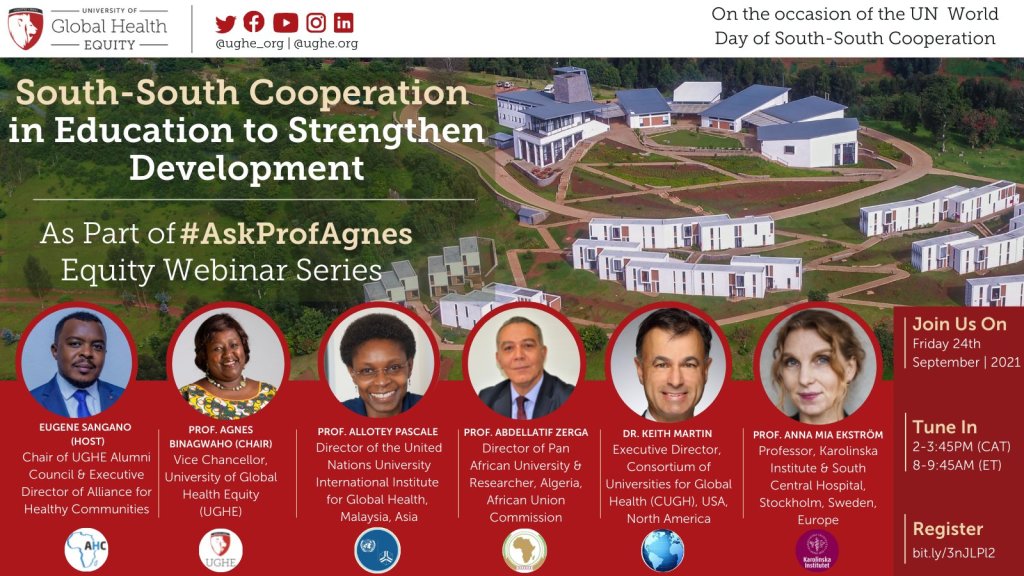
As a monthly continuum of the equity webinar series, I invited a panel of leaders to discuss the role of South-South Cooperation in education to strengthen the development of the Global South. The panelists included: Prof. Allotey Pascale, Prof. Abdellatif Zerga, Dr. Keith Martin and Prof. Anna Mia Ekstrom.
In the month of September, the United Nations commemorated the International Day of South-South cooperation which is aimed at raising a more inclusive, resilient and sustainable future for the globe as it responds effectively to COVID-19. In this month’s equity webinar series, the panelists discussed on the engagement of higher education institutions in promoting education through South-South Cooperation, the role of the African Union in improving education through South-South cooperation, how the western world can support Education South-South Cooperation and example of Sweden and the role of the CUGH in improving education by supporting South-South Cooperation.
In my remarks, I recalled on the need to increase South-South partnerships to help achieve SDG’s “South – South partnership should also help us to respond to challenge of retaining qualified professionals and skilled people in the global South.In pushing towards this agenda, to bridge gaps of education and skills in Africa, there is a clear need for more South-South cooperation to create
synergy and accelerate our journey to achievement the SDGs”

Overall, together we brought attention to the work being done to increase momentum for South-South Cooperation and the right way of collaborating and supporting these partnerships.
Read more:https://www.youtube.com/watch?v=2GPnpne6v7g
Connected Women Leaders Conference
September 18,2021

I was invited by the Connected Women Leaders to attend the conference to discuss the current state of the world as it relates to women and to 3 of CWL’s main pillars: Global Health, Climate Justice, and Food Security. In my talk, I highlighted the lessons from LMIC COVID-19 response, the activities in which I am involved to champion global health equity such as the first conference on public health in Africa (CPHIA). I also talked about UGHE response to COVID-19 including 100% vaccination for all UGHE staff, faculty and students as an example to changing vaccine inequity.
Brookings Institution- Panel onAccelerating COVID-19 Vaccinations in Africa
September 15, 2021

I was invited by the Brookings Institution to participate on a moderated panel on Accelerating COVID-19 vaccinations in Africa.The Brookings Institution is a nonprofit public policy organization whose mission is to conduct in-depth research that leads to new ideas for solving problems facing society at the local, national and global level.
In my discussion I stated the following:
“We all know that vaccine inequity not only harms countries in Africa but will eventually bounce back and harm the US and Europe as more dangerous and inevitably vaccine-evading variants emerge”
“High-income countries that have and still continue to unnecessarily store more vaccines than the quantity they need to vaccinate their entire populations, some for as much as five times over, need to they immediately need donate their surplus vaccines to the COVAX initiative”
“We need to stop talking about vaccine hesitancy on the African continent when 80% of the population is willing to get vaccinated but only 3% have had access.”
“We need to develop ourselves as Africans the vaccine manufacturing capacity”
WHO World Patient Safety Day is “Safe Maternal and Newborn Care”
September 15, 2021

I was invited by Harvard T.H. Chan School of Public Health to be a panelist in celebration of World Patient Safety day on this year’s theme “Safe Maternal and Newborn Care”. I spoke on some successful strategies for improving maternal and newborn safety you have seen in Rwanda. In my discussion I mentioned how Rwanda mitigated to reduce maternal and newborn mortality during the pandemic which was achieved through our national strategic plan, by training CHWs to sensitize citizens on preventative behavior, through consistent data reporting, through the commitment to equality, through decentralization of the healthcare system, by having mass campaigns, through the horizontal primary health care systems improvement and through rapid adoption and innovation.
Watch full video here: https://www.youtube.com/watch?v=MTQuJT7lWRM
AfriPEN Conference-What should change in Health Sciences education in Africa to reach the SDGs?
September 15, 2021

I was invited by the Africa Interprofessional Education Network to be a keynote speaker for the 3rd AFRIPEN conference. AfriPEN is a consensus -based partnership between various institutions and individuals with the vision to establish interprofessional education and collaborative practice(IPECP) as an integral part in training the health workforce and the effective functioning of systems for health in sub Saharan Africa.
In my talk I discussed changes needed in education to improve the number and quality of the healthcare workforce in Africa, to improve health outcomes and ultimately achieve the SDGs. I provided the overview of challenges facing the African health workforce, including effects of the COVID-19 pandemic on health education;I discussed the role of universities in achieving the SDGs; I provided recommendations and success stories in Africa towards health education strengthening; and gave an example of IPECP at UGHE.
Friends of Europe-Balancing values and relationships: Has multilateralism worked in favour of fairness or is it about balancing national budgeting?
September 9, 2021

I was invited by Friends of Europe to be a panel speaker for the European Young Leaders Seminar along with Pascal Lamy (President Emeritus of the Jacques Delors Institute and Friends of Europe Trustee). European Young Leaders programme is a unique, inventive and multi-stakeholder programmes that aims to promote a European identity by engaging the continent’s most promising talents in initiatives that aim to shape Europe’s future . In my discussion, I recalled examples of Europe’s failure to show global solidarity through vaccine distribution inequalities where they are hoarding doses and lack of following the science.
“This Notion of solidarity should be the foundation of the relationship between Africa and Europe and be embedded with mutual respect”
During the Q&A session, I talked about what colonialism represent for the current state of the African-European relations, COVAX mechanism and the Chinese and African partnership.
UNU-WIDER-COVID-19 and Development Effects and New Realities for Global South
September 8, 2021

I was invited by the UNU-WIDER to discuss on the future global health governance as a panel speaker along with Dr. Obi Bojiofor (Former Deputy Director of UNU International Institute for Global Health and Adjunct Research Professor at Carleton University)and Dr. Roberta Andraghetti (PAHO Regional Advisor on International Health Regulations).The United Nations University World Institute for Development Economics Research (UNU-WIDER) provides economic analysis and policy advice with the aim of promoting sustainable and equitable development for all.
The aim of this panel session was to reflect how the crisis of COVID-19 was handled and the lessons to learn from. In my discussion, I talked about the three major lessons which is to make health the center of all development, finding ways to bridge social-economic inequities especially for the vulnerable people, lack of solidarity and push resilience. I also highlighted that regional governance can only be relied by institutions like Africa CDC to respond to such global crisis because they are supported by head of states.
Tortoise Platform-The Arms Race: How many more people will die from COVID-19?
September 6, 2021

I was invited by the Tortoise Platform to be a panel speaker to discuss Global Vaccine Inequality, and the race to vaccinate low income countries.Tortoise Platform is a media platform that provides events analysis rather than breaking news. Its main objectives are chasing a story rather than news, and addressing the power gap between the powerful and powerless.
In the conversation, I highlighted that global vaccine inequality is highly due to HIC hoarding doses, the lack of regulation of prices for vaccines doses from private vaccine manufacturing firms which puts in detriment low income countries. I also discussed on what is needed to change the situation, which is to call for immediate action to HIC to supply and contribute to global vaccine access through COVAX because the surge of variants will threaten the lives of those who are not vaccinated.
Stanford University-INFODEMIC: A Stanford Conference on Social Media and COVID-19 Misinformation
August 26, 2021

I was invited by Stanford University of Medicine to be a panel speaker to discuss on vaccine hesitancy along with Dr. Gloria Giraldo and Dr. Aida Habtezion. During my talk, I highlighted that in lower and middle income countries (LMIC), vaccine hesitancy is not a pressing challenge but rather equitable vaccine access. I talked about the reasons behind vaccine hesitancy, which is the lack of trust in the healthcare systems, in science, government or security system.
“Trust is a big social determinant of health, trust in the health system should be built on a day to day basis not during crisis”
I also mentioned that if there is a history of mistrust and people in charge do not take accountability, hesitancy is bound to be greater.
In addition, I mentioned that the pandemic was mismanaged because all the solutions were not global and were full of greed from the high income countries.
“A global problem requires a global solution”
Lastly, I mentioned that vaccine manufacturing capacity should be increased in Africa to avoid being last served.
Watch Full video here:https://stream.mux.com/wqXaLy5HLvSmwh6lryY3oxzCAZsGwtmt/high.mp4\
UGHE-#AskProfAgnes Equity Webinar on Global Humanitarian Efforts during COVID-19
August 26, 2021

As a monthly continuum of the equity webinar series, I invited a panel of leaders in the humanitarian network to discuss global humanitarian efforts during the pandemic and raise awareness for the challenges faced by displaced people and to commemorate a UN World Day. The panelists included: Dr. Jonathan Calbayan, Dr. Sheila Davis, Dr. Jemilah Mahmood and Ms Rita Amukhobu.
In the month of August, the United Nations commemorated the World Humanitarian Day and we used this platform to bring awareness of the current state of refugees and how humanitarian actors are playing their role to improve their living conditions through funding, aid work support and policy. In this month’s equity webinar series, the panelists discussed on the humanitarian role of NGOs, the role of UNHCR, the successes and challenges of humanitarian activities by national societies all during the COVID-19 crisis and the role of the African Union during humanitarian crises example of COVID-19 pandemic.
In my introductory remarks, I highlighted that: “If we do not act through coordinated efforts in global assistance to support context-specific solutions in countries affected by humanitarian crises, there will be a huge risk that COVID-19 and its variants will ravage vulnerable populations of displaced persons, continue to spread across borders, and threaten global health security”
Overall, together we brought attention to the work being done by humanitarian workers, the right approaches to fight the unprecedented effects of COVID-19 to protect vulnerable communities and stated a clear role for each humanitarian actor in this fight.
Watch Full video here:https://www.youtube.com/watch?v=tx_qXB1Tz6o
Graduation UGHE-MGHD Class of 2021
August 22,2021

On Sunday August 22, we celebrated the 23 cohort members of the UGHE Masters in Global Health Delivery program from 12 countries for completing their academic course. We were joined by distinguished guests including the Head of Africa CDC (Dr. John Nkengasong), the Rwandan Minister of Health (Dr. Daniel Ngamije) and the Rwandan Minister of Education (Dr. Valentine Uwamariya) who also gave students their remarks. During the ceremony, I took the opportunity to give short remarks to the students.
“Today dear students, you are graduating, you are now fully integrated in the alumni family and the global health network as our colleagues. Your passion for equity brought you to UGHE and during the past year you have been equipped with the theoretical knowledge and the implementation skills to contribute constructively to this mission”
“To prepare you for this engaging work, UGHE has equipped you with the required tools to be advocates of inclusive holistic systemic change, with leadership and managerial skills to help you improve, create and lead health systems to improve the lives of all, leaving no one out”
“As I conclude, my wish is that you take away from UGHE, the fruitful discussions, enlightening talks, incredible experiences with your peers, as well as the networks built with your fellows and other members of the UGHE family whose efforts have forged you into high-caliber graduates and great global health leaders”
Watch full video here:https://www.youtube.com/watch?v=E_99Qxjdbdo
UGHE-Global Health Summer Bootcamp Closing Session
August 13, 2021

After 9 weeks of training, the Global Health Summer Bootcamp interns concluded their course program. In my closing remarks I highlighted the following:
“We have observed your growth through the excellent research presentations, through your weekly reports submission, through your active engagement during discussion on readings, and through interactions with the guest speakers. Overall, your positive participation revealed your willingness to learn and careful preparation of this program.”
“I hope that what you have learned here through this experience will help you a lot in your current studies, future careers, and lead to the development of the region in the future.”
UGHE-Global Leadership In Nursing And Midwifery
August 9, 2021

At the University of Global Health Equity, we inaugurated the executive program for Global Leadership in Nursing and Midwifery, which is a step stone for the nurses and midwives who are the pillars health delivery.
“Nurses and midwives play a crucial role in the delivery of healthcare but they must be trained in leadership at the highest level so that they are able to strengthen their vital roles in healthcare service delivery to the decision makers, which could help for vulnerable populations in Africa to receive quality healthcare, and equitable access”
“Mobilizing the political will to improve the health, well-being, and safety of patients, building on your critical thinking, problem solving and disaster management skills, and mitigating the shortage or rather lack of equitable distribution of nurses and midwives in many countries, are just some of the ways in which we can reaffirm, protect, and leverage the work of nurses and midwives through attaining leadership roles”
“With this program, you will become professionals strengthened in deliberate financial investment, effective legislation, regulation, education and employment practices, along with the deep understanding that there needs to be a fundamental shift in policy at national and global levels towards equitable access to healthcare services, and a skilled, empowered nursing workforce will help build a stronger, more resilient health system”
For more information on executive education programs offered at UGHE email: exec_edu@ughe.org
UGHE Masters in Global Health Delivery-Class of 2022 Orientation
August 9, 2021

At the University of Global Health Equity, we welcomed a new cohort for the Masters program in Global Health Delivery. I delivered an orientation speech to give the students insight on what to expect from being a “Lion” and being enrolled as an MGHD student. I also gave a brief overview of UGHE’s mission, values and vision.
“UGHE’s uniqueness is that it is pioneer in equipping global leaders with training that helps to provide essential health care services to neglected communities, with critical thinking to solve some of the most complex global health issues and with tools to build stronger equitable health systems”
To learn more about this Masters program follow this link:https://ughe.org/academics/mghd/
Stellenbosch University-Women’s Day
August 5, 2021

I was invited to be a keynote speaker for the Women’s Day celebration at Stellenbosch University. I discussed the state of women’s issues worldwide and potential solutions. In my talk, I highlighted that gender equity is critical for financial improvement, business performance and results in improved health outcomes. In order to achieve that gender equity we need to implement better clinical practices, increase female representation in health positions of management, promote collective action between men and women for institutional change and provide capacity building with training and mentors fir women. I gave the example of Rwanda for achieving gender equity, through the establishment of a legal framework that ensures gender equity, a gender budgeting agenda and increased opportunities for women. Finally, I mentioned what my university is doing to achieve gender equity, where we have 70% women enrolled as medical students and 50% in other courses.
4th Annual AFREhealth Symposium
August 4, 2021

I was invited for the 4th Annual AFREhealth Symposium by AFREhealth to discuss the global view on social accountability in higher education. The African Forum for Research and Education in Health (AFREhealth) is an interdisciplinary health professional grouping that seeks to work with Ministries of Health, training institutions and other stakeholders to improve the quality of health care in Africa through research, education and capacity building. It is a conglomerate of individuals, institutions, associations and networks from all the geographic and linguistic regions of Africa namely Anglophone, Francophone, Lusophone and Arabophone.
In the panel discussion, I focused on building social accountability into global health education, using the example of my university, the University of Global Health Equity. I also brought attention for five factors in building social accountability in global health education: building human resource capacity according to the burden of disease; ensuring equitable access to quality education; fostering a continuous sense of curiosity; educating on the vicious cycle of poverty and diseases and the social determinants of health; and equipping students with the practical skills needed to repair, create and manage systems.
UGHE-2021 Global Health Summer Bootcamp
July 28, 2021

As a yearly continuum, UGHE hosts a Global Health Summer Bootcamp with interns around the world. The bootcamp is aimed at developing young global health leaders to get a better understanding of equity in health systems building and health care delivery.
I talked about the Architecture of Global Health with a focus on access to health for internally displaced people and refugees worldwide.
I shared how to examine the needs of the displaced people and response to this crisis and the fact that “No matter where you are in the world, refugees and displaced people are the most vulnerable”.
In Rwanda, Mahama camp, is one of the largest camp in Rwanda with available housing and health posts and other services. There is an effort to vaccinate children of refugees as the country vaccinate Rwandan children and CBHI is available to refugees living out of the refugee camps as well as education opportunities from primary level inside the camp to secondary schools outside the camp.
For stopping the spread of COVID-19 refugees above 60 have been vaccinated, as they are the most at risk.
“You shouldn’t believe that refugees in Europe are all in decent conditions, the conditions of refugee camps demonstrate that the level of development of a country does not ensure refugees receive decent human good care. Like all over the world it deepens depending on the political will.
Other communities not having fixed place to live face exclusion such had Gypsies in Europe who are unfairly treated yet they are born and live in Europe since centuries. I also gave an example of community exclusion in USA where studies have shown that your life expectance is highly related to your zip code and not as commonly only admitted to you genetic code.
Harvard Global Health Delivery Intensive (GHDI) Program Graduation
July 23,2021
As a Senior Lecturer for the Department of Global Health and Social Medicine at Harvard University, I was invited to give a keynote speech for the Harvard Global Health Delivery Intensive Program Graduation.The program aims aims to organize the study of health care delivery and to stimulate collaboration among educators, researchers, stakeholders, and implementers while building capacity in health care.
In my speech, I highlighted on the role of health professional education/global health education in the fight for global health equity:
“If we build health facilities in all corners of a country, we avoid the risk that an individual living in a remote area will not have access to care on time but we need a holistic approach tackling all inequities in quality and quantity such as transport, language. Having infrastructure is not enough and when you discover new causes and sources
of inequities tomorrow, you need to be ready to fight”
“The COVID-19 pandemic has shown us that failure to protect health as a human right for all globally can have disastrous impacts across all sectors of society and now across humanity because by not having successfully stopped the spread of the virus worldwide. Due to lack of vaccines for the developing world we have increased the risk for all to face a variant that does not respond to the current vaccines, putting all in danger and showing that no one will be safe until we are all safe. Global health relies on understanding and addressing all vulnerabilities”
“A crucial component of global health is teaching by example. Now it is your turn to be the role models. The world needs good models”
“I hope that this Global Health Delivery Intensive program has equipped you with the knowledge
and skills necessary to join the builders making global health equity a reality.”
NIHR-UK-Global Health Implementation During The COVID-19 Pandemic
July 15, 2021

I was invited for the 4th UK Implementation Science Conference as a panel speaker to present on Rwanda’s COVID-19 response using Implementation Science. The conference brings together online researchers, policymakers, clinicians, practitioners and service users from around the world and this year’s theme was on “Supporting the pandemic response? Implementation science in the time of COVID-19”.
In my talk, I highlighted on the fact that Rwanda was ranked 6th for successful implementation to COVID-19 response. This success was due to the following: understanding the Rwandan context, identifying the weaknesses, adopting innovations, maximizing available resources and early preparedness for vaccine distribution.
UGHE-#AskProfAgnes Equity Webinar on Safe Blood and Save Lives-Driving Awareness of Blood Donation
July 14,2021
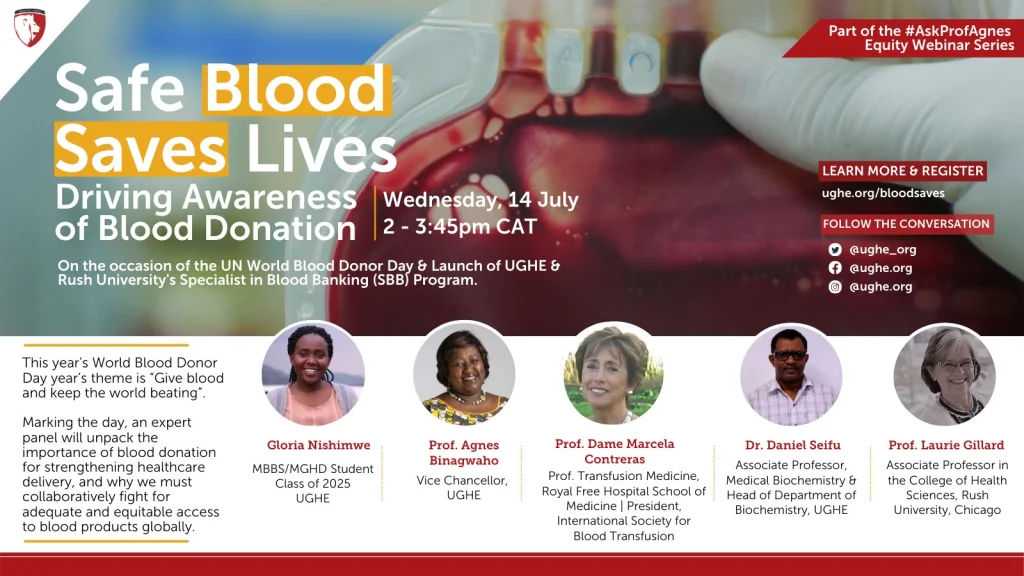
As a monthly continuum of the webinar series, I invited a panel of prominent leaders and experts to discuss safety for blood donations, and raise awareness for the global demand for blood supply and to commemorate a WHO World Day. The panelists included: Prof. Dame Marcela Contreras, Prof. Laurie Gillard and Dr. Daniel Seifu. In the month of June, the World Health Organization commemorated the World Blood Donor Day and we used this platform to bring awareness to what the current situation of blood supply and donations are and the proposed solutions in their regions are. In this month’s equity webinar series, we discussed the impact of COVID-19 on blood supply in the United States, sufficiency and safety of blood donations, blood transfusion and supply specifically in Sub-Saharan Africa, the existing needs, challenges, and way forward.
We brought attention to the world in reinforcing efforts in voluntary donation, and use campaigns to raise awareness, encourage young people and adults to take part in the movement and create training opportunities to ensure safety for blood donation. During these challenging times, now more than ever, donating blood can save many lives, hence ensuring that the community understands the value of this act is fundamental to increasing the global blood supply especially for countries experiencing shortages.
Watch full video here:https://www.youtube.com/watch?v=7WdUCFSH_bU
2021 Fogarty Global Health Fellows and Scholars Orientation
July 12, 2021

I was invited by the 2021 NIH Fogarty Global Health Fellowship Program to give the “Charlie van der Horst Memorial Lecture” on How to Give your Elevator Speech. The current program supports six U.S. university consortia to provide one (1)-year mentored global health research training opportunities to predoctoral/pre-professional and postdoctoral/post-professional trainees from the U.S. and low- and middle-income countries (LMICs) at established research institutions and project sites in LMICs. I gave the fellows and scholars advice on how to prepare, design, and perfect an elevator speech. For a good elevator speech, I highlighted that it is important to identify the context, the challenges and gaps, available resources, the needs and demands. I also noted that it is important to have your data and arguments ready, to understand your audience, to know your strengths and weaknesses and always be ready.
Global Health Corps -Global Health Training Institute
July 12,2021
I was invited by the Global Health Corps as a guest lecturer to discuss on Global Health Leadership using the example of Rwanda. The Global Health Corps is an organization that is dedicated to catalyzing systemic change towards greater diversity, equity, and inclusion in the global health sector. In my lecture, I discussed on the history and demographics of Rwanda, where I highlighted that 18% of the population live in urban areas which shows that majority of the population lives in rural areas. I also noted on post-genocide health outcomes where the rapid transformation was due to the improvement in life expectancy, decrease in infant mortality, reduction in child labor mortality and reduction under 5 children mortality. Lastly, I deliberated on the key players and success factors that played a role in strengthening the Health system in Rwanda and contributed to better health outcomes.
EuroScience policy forum-The implementation challenge
June 30, 2021

I was invited for the 1st EuroScience policy forum to discuss on the implementation challenge. The 1st EuroScience Policy Forum was discussing on the changes in societal expectations on academic institutions and identify potential new pathways to a more sustainable academia in the future. In the panel discussion, I argued that funds for implementation science is not the main issue, rather identifying the needs, developing strategies to facilitate implementation science and to apply it according to the needs. In addition, creating cost-effective solutions for decision-makers, using evidence-based strategies, interventions and policies to enable better health-outcomes.
Health Data Research UK’s fourth Annual Scientific Conference
June 23, 2021

I was invited for the Health Data Research UK’s fourth Annual Scientific Conference to chair a session on what was COVID-19 response from countries of Rwanda, Norway and Singapore. Health Data Research Annual scientific Conference is an event showcasing the latest advancements in health data science. I talked about the overview of Rwanda’s COVID-19 response, which was addressed by having an equitable approach, adoption of interoperable innovations, having rapid response readiness and preparedness for vaccine distribution.
Watch full video here:https://www.youtube.com/watch?v=U1H_16oTBkg
Project Syndicate on Pandemic Preparedness
June 23, 2021

I was invited by Project Syndicate for a panel discussion on “Preventing the Next Pandemic”. Project Syndicate is an international media organization that publishes and syndicates commentary and analysis on a variety of global topics. In the discussion, I stated that despite what is the common belief for why Africa was able to manage COVID-19 better than other stronger health systems, the reason being of the Ebola outbreak in Western Africa is totally wrong, but rather because African countries followed science and common knowledge on how to manage epidemics using evidence-based interventions. I also emphasized on the lack of political leadership, lack of accountability and lack of trust in scientists as the reasons of failure for preparedness for the pandemic in rich countries contrary to what was achieved in Africa.
Watch full video here:https://www.youtube.com/watch?v=x9uUX3bG18s
RCPCH-Impact of COVID globally on achieving the SDGs
June 16, 2021

I was invited to be a speaker for the 2021 Royal College of Paediatrics and Child Health conference. This conference gathers globally professionals in the paediatrics community to indulge in discussing the latest research and innovations in the field. The theme of the conference for this year was on “Challenges, opportunities and solutions for child health in the COVID-19 era“. In my talk, I emphasized that children were the hidden victims of the pandemic because it had a negative impact on their mental health, social lives, education and economic wellbeing. It also aggravated the social economic disparities, where parents that fell into poverty posed a heavy burden on their children.
Kofi Annan Global Health Leadership Fellowship-Keynote address: Building Back Better- The experience of Rwanda
June 15, 2021
I was invited by Kofi Annan Global Health Leadership Fellowship to give a keynote address as a member of the advisory committee of the Africa CDC- Kofi Annan Global Health Leadership Program. The Kofi-Annan Global Health Leadership Program has a goal to support senior African public health leaders acquire advanced skills for leading transformation of public health leadership in Africa. I shared on the experience of Rwanda, specifically on how to build a strong health system integral to the priorities and needs of the country. I explained the journey of Rwanda, as a country that rose from a genocide, where hospitals and the health system were completely decimated to now a country with a universal health care plan, teaching universities including my university, University of Global Health Equity that are all contributors of the restoration of the Rwandan Health System.
National Institute Health Research UK Global Health Research Training Forum
June 10, 2021

I was invited to speak as a panelist for the National Institute Health Research (NIHR) Academy to speak as a panelist for their third annual Global Health Research Training forum.The Global Health Research Training Programme supports the training and career development of researchers. During the panel discussion, the main message I conveyed was how critical it is to have platforms such as the training forum that involve lower middle income countries (LMIC) researchers to participate. Therefore, it is important to note that investing in researchers of LMIC without providing landing platforms prevents retention of trained researchers and can only further contribute to brain drain.
St. Luke’s Medical Center -The Future of the Hospital
June 9, 2021

I was invited by St. Luke’s Medical Center College of Medicine to discuss on the critical importance of hospitals as we continue to face the pandemic. I mentioned that at my university, the University of Global Health Equity we use a community-based teaching approach and stress the relevance of this system, which demystifies the function of physicians and encourages them and hospitals to be used for more complex issues.
Watch full video here:https://fb.watch/6-rUy7Dc_7/
GZERO-Stronger Partnerships for a Healthier World
June 5, 2021
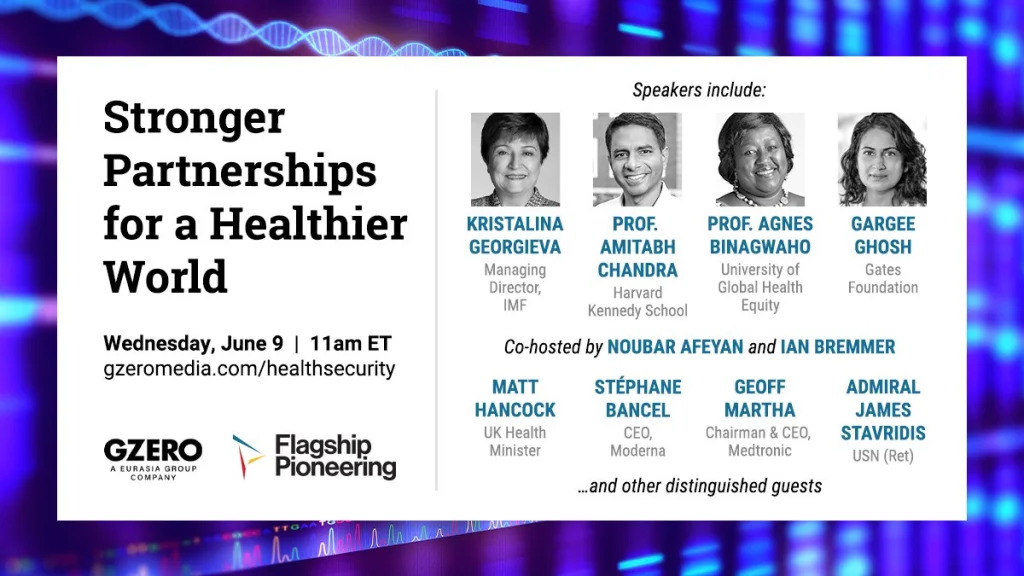
I was invited to be a panel speaker by GZERO to discuss preparedness for the next pandemic. GZERO is an Eurasia Group media company dedicated to cover global affairs. During the live discussion, I discussed on how multilateral efforts to distribute vaccines were not as successful as it had been anticipated. Although, efforts made were global, as far as Africa was concerned, the two main contributors of vaccine distribution were only from India and China. In addition, I noted that since COVID-19 pandemic has been marked as a threat to the lives of people and economies, global efforts should have been focused on solidarity, cleared a triple-waiver and accelerated rapid knowledge transfer. Lastly, I highlighted that vaccine manufacturing should be considered to be locally made anywhere on the African continent to avoid Africa being the last served.
Watch full video here:https://youtu.be/Ab3AnDP7oCk
Mo-Ibrahim Foundation-Lessons from the pandemic: an urgent call to strengthen Africa’s health capacities
June 3, 2021

I was invited to be a panelist for the Mo-Ibrahim Foundation Governance weekend platform to discuss ways of strengthening Africa’s health systems capacities. The Mo- Ibrahim foundation is a foundation created to focus on the critical importance of governance and leadership in Africa. In the forum session, I highlighted that Africa’s ability to ramp up its vaccine manufacturing capacity and the independence in vaccine supply is a matter of security for the continent but also a matter of focusing on Africa’s innovation strategies that are already in use.
Watch full video here: https://www.youtube.com/watch?v=OibJvAn5c5A&list=PLfdHh52XxPRNZlLpnCVMQ21QFSW2X3jlg&index=7
Graduate Institute of Geneva -Women Power, Politics and the Pandemic: Celebrating Women’s Leadership
May 28, 2021

I was invited as a panel speaker by the Graduate Institute of Geneva and Global Health Centre for the World Health Assembly 74: Women Power, Politics and the Pandemic: Celebrating Women’s Leadership. The assembly shed a light on the current global crisis by leading a discussion with women experts in health and other social issues.In my talk, I highlighted that when a country invests in women, increases their representation in leadership roles, it amplifies development and community engagement of the country.In addition, women play an instrumental role in making positive difference, it is therefore vital that women are supported through education and human rights.
Watch full video here:https://www.graduateinstitute.ch/WHA-Women
University of Maryland Baltimore-Decolonizing Global Health Education
May 26, 2021

I was invited by the University of Maryland Baltimore to discuss and to advocate for decolonizing global health, in particular global health education. During the discussion, I deliberated on the systemic failures in global health education that perpetuate inequitable access to health education and to health service delivery. I discussed the obligation of institutions in high-income countries to reevaluate their countries’ and their institutions’ history and their approach to education in order to challenge biases that we are taught from the first drop of milk. I emphasized the importance of decolonizing funding for research and acknowledging and equally compensating for the output of research done by African scientists. I provide the work of UGHE as an example of an institution that continually strives to decolonize global health education.
Watch full video here:https://www.youtube.com/watch?v=04cTspTqxKw
UGHE-#AskProfAgnes webinar series: Recognizing Biodiversity as a Public Good
May 25,2021

As a monthly continuum of the webinar series, I invited a panel of prominent leaders and experts to discuss biodiversity, climate change, and raise awareness of environmental justice. The panelists included: Prof. Mary Robinson,Dr. Philip Landrigan, Dr Phaedra Henley, Dr. Elvis Paul Tangem, and Kate Harriden. In the month of May, the United Nations commemorated the International Day for Biological Diversity and we used this platform to bring awareness to what the current situation of biodiversity loss is and the proposed solutions in their regions are. In this month’s equity webinar series, we discussed the foundation of biodiversity explained by life on Earth, the different species, and ecosystems that make up the biosphere as well as its habitats, environment or places in which they exist.
We brought attention to the fact that the international community is urged to stand in solidarity for the adoption of a new global biodiversity framework that will address climate, health issues, and food and water security to ensure sustainable livelihood of which biodiversity is a foundational aspect. As humans, we are dependent on the biosphere and we must recognize the value and needs of all its species because they all provide us with what is essential for our everyday functioning. We all know that the global issues we face are linked to diversity, and it is time to recognize that biodiversity decline requires urgent global, and local multi-sectorial actions to halt it and reverse it.
Watch full video here: https://www.youtube.com/watch?v=F3ZG-xxeYkE
Africa Europe Foundation, ‘Talking Africa EU Series’: “Nobody is safe until everyone is safe.” A test of solidarity or the catalyst for Europe and Africa to do things differently?
May 20, 2021
As Co-Chair of the Africa Europe Foundation Strategy Group on Health, I joined Gunilla Carlsson, Co-chair of the Africa Europe Foundation Strategy Group on Health and Tamsin Rose, Senior Fellow at the Africa Europe Foundation to discuss the how Europe and Africa can work together to overcome vaccine inequalities. This discussion was part of the ‘Talking Africa EU series’ that promote “a ‘whole of society’ approach, allowing key stakeholders from both continents to share perspectives on the future of the relationship.” In this debate, I discussed the problem was not lack of capacity and resources but rather the lack of willingness to work together and lack of trust in Africans.
Watch full video here: https://www.youtube.com/watch?v=TqO8NoR3o_I&t=912s
IFMSA (International Federation of Medical Students Association) Youth Pre-World Health Assembly
May 19,2021
I was invited to participate in the IFMSA (International Federation of Medical Students Association) Youth Pre-World Health Assembly that discussed on Science, Research, Innovation, Bioethics and Decolonizing Global Health. In particular, my talk was focused on the robust and exemplary response of the government of Rwanda that was shown during the pandemic including the initial lockdown strategy, channeling the potential of community health workers, HIV & AIDS management, and immunization routines.
Körber History Forum 2021: Corona and Humanitarian Law
May 19, 2021
I was invited to join this the 2021 Körber History Forum. This year’s forum’s motto motto– putting crisis in context brought together esteemed speakers from around the world to discuss how we connect the dots between history and politics. I spoke on the panel titled “Körber History Forum 2021: Corona and Humanitarian Law” alongside Armin von Bogdandy, Mark Honigsbaum and Sven Stockrahm. On this panel, we discussed global health equity between human rights, national interests, and weakened multilateralism. I shared about the importance of accountability among politicians and their responsibility around scientific information as well as budgeting. More importantly, Global Health Equity is centered about human rights with a focus on the most vulnerable.
Watch full video here: https://www.youtube.com/watch?v=TKhyIzBBxvQ&list=PL21YiU8i5e4GMS33_ZPOjYP_iQaZO4Cub&index=5
Africa Europe Foundation-Sahel Renaissance: Enabling a Just Rural Transformation
May 12,2021

As co-chair of the Africa Europe Foundation Health Strategy group, I joined the discussion panel to discuss how Africa and Europe seek to re-set their partnership for the acceleration of sustainable development on both continents and need to work together to find solutions posed by the COVID-19 pandemic and the climate crisis. In this debate, I insisted that a call for action is required for the restitution of local resources owned by European countries as a result of colonialism, so that African countries can regain back their resources and have the chance to exploit them more.
Watch full video here: https://www.friendsofeurope.org/events/the-sahel-renaissance-enabling-a-just-rural-transformation/
Planetary Health Alliance and University of São Paulo: Planetary Health, Transdisciplinarity, and Academic Careers: new structures for a new science and education
April 27, 2021

I was invited by the Planetary Health Alliance Director, Dr. Sam Myers and Dr. Antonio Mauro Saraiva, 2021 Planetary Health Annual Meeting Chairman to be a panelist at the 4th Planetary Health Annual Meeting aiming to bridge communities to achieve the Great Transition by highlighting collective planetary health values; showcasing change-making science, stories, solutions, and communities; and building systemic solutions across economics, governance, and civil society. On the panel titled: “Planetary Health, Transdisciplinarity, and Academic Careers: new structures for a new science and education” I spoke about the importance the interlink between human health, the environment and the health of our planet. I also talked about the role of the University of Global Health Equity (UGHE) as an academic institution that is training the next generation global health leaders and professionals who are ready to not only deal with the clinical and medical consequences of environmental outcomes but also advocate and implement socioeconomic policies that are favorable to the health of their communities, and the planet.
Watch full video here: https://www.youtube.com/watchv=VNZ2i5D0UaQ&list=PLptcPrw0lc4qq2teRSjvC0P6GFo9KVnTC&index=3
Skoll World Forum on Social Entrepreneurship: Cultivating System Leaders for an Age of Pandemics
April 14, 2021

On April 14, I participated in the 2021 Virtual Skoll World Forum convened by the Skoll Foundation. I was invited by Dr. Peter Drobac, Director, Skoll Centre for Social Entrepreneurship to speak on a panel session titled “Cultivating System Leaders for an Age of Pandemics.” During this session, I first shared about Rwanda’s response to the COVID-19 pandemic based on strong leadership, compassion, and following the equity agenda. I also discussed some of the problems with leadership which include leaders that do not make decisions based on science but rather self-gain and the rise of nationalism. In order to create system leaders, we need to teach young leaders that each and everyone is a leader. At UGHE, we are educating future global health leaders who are equipped to leadership and management skills that are crucial to create, improve and maintain equitable, resilient systems, but this kind of leadership is based on humility and compassion.
Watch full video here: https://www.youtube.com/watch?v=NIWBILj_Els
Watch videos from other sessions here: https://skoll.org/2021-skoll-world-forum-closing-the-distance/
University of Global Health Equity: Equity in Vaccine Rollout: Challenges and Solutions
April 12, 2021
I joined a great discussion alongside global health leaders from UGHE and Partners In Health (PIH) including; UGHE Chancellor & PIH Co-Founder & Chief Strategist, Dr. Paul Farmer; Director of the Skoll Centre for Social Entrepreneurship, Dr. Peter Drobac, Vice Chairman and Partner at Global Infrastructure Partners & and PIH Co-Founder, Dr. Jim Yong Kim. The conversation titled: “Equity in Vaccine Rollout: Challenges and Solutions” was moderated by PIH’s CEO, Dr. Sheila Davis. On this panel, we discussed how COVID-19 has exacerbated existing inequities in health and health delivery and how the vaccine roll-out has become tied to a damaging nationalism. I shared with the audience the importance of equity agenda and global solidarity in the vaccine roll out with a focus on the developing world.
Watch full video here: https://www.youtube.com/watch?v=hxyuS1JP1qc
8th Annual Women Working for the World Foundation: “Gender Equity: A Pillar to Rebuild a Nation”
April 8, 2021
As part of the Annual Women Working for the World Foundation, I was interviewed by Marcela Prieto, Political Scientist from Los Andes University (Bogotá-Colombia) as part of the Women Working for the World organized by Catalina Escobar and the Juanfe Foundation. In this interview, I discussed women empowerment, gender equality, and shared my experience and my role in building an equitable health system in Rwanda. I also shared about Rwanda’s journey to forgiveness especially highlight the role Rwandan women played to contribute to the rebirth of the nation.
Watch full interview starting at 4:46:00: https://www.youtube.com/watch?v=_1dlpR6ERbw
Liu Institute Network for Africa (LINA) at the University of British Columbia: “The Power of the African Woman: An Epitome of Resilience, Intelligence, and the Bedrock of Development”
March 31, 2021
On March 31, I participated in Liu Institute Network at the University of British Columbia School of Public Policy and Global Affairs for their webinar series “African Women’s Leadership: Resilience, Intelligence, and the Bedrock of Development.” I spoke on the panel entitled “Women Shifting the Health Landscape in Africa” was moderated by Dr. Neo Tapela and was joined by Professor Tlou Sheila. On this panel, I shared my experience and journey to becoming a global health leader and my long-term commitment to fight against gender and health inequities. I called upon the audience to use their positions of power to empower women and use their positions to advocate for a change in laws in order to ensure sustainable change. I reminded the young women in the room that nothing can stop them because the limit is not sky nor is it the universe.
Watch full video here: https://www.youtube.com/watch?v=exe4Og9F1rA&t=13s
Venice Forum: Why investing in Maternal, Newborn and Child Health (MNCH) is critical for sustainable recovery after COVID-19
March 23, 2021
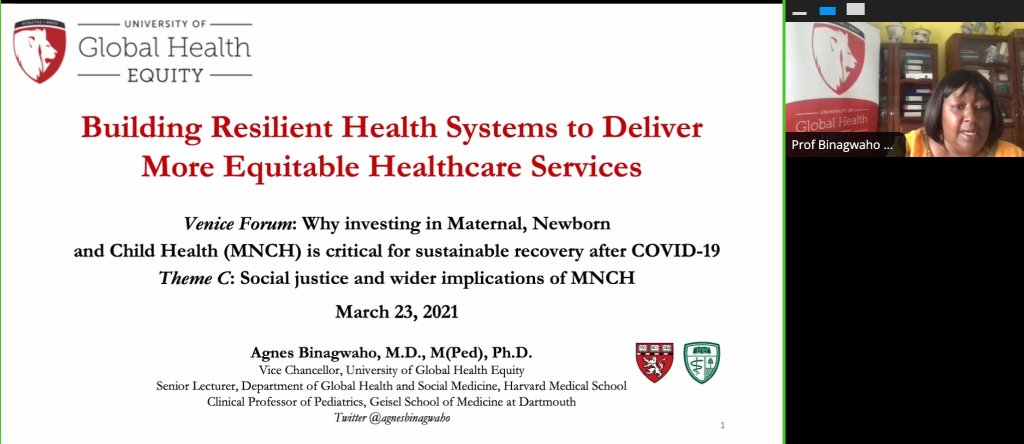
On March 23, I was invited by the Venice Forum organizing board to participate on a panel session titled “Social justice and wider implications of MNCH.” In my presentation titled: “Building Resilient Health Systems to Deliver More Equitable Healthcare Services,” I highlighted that pregnant women, newborns, and children under five are the most vulnerable citizens around the world. However, majority of maternal and child deaths are preventable. It is imperative that we create health systems that provide affordable and quality healthcare without leaving anyone behind. Giving Rwanda as an example, I discussed the decentralized system that has been built through Community Health Workers (CHWs) to meet mothers and children where they are. When strong systems are in place, they are resilient to health threats such as the COVID-19 pandemic. However, to ensure that we continue building resilient health systems, we need to provide quality global health education that allows health professionals to provide equitable health care.
learn more: https://www.fisv.org/wp-content/uploads/2021/03/Comunicato-stampa.pdf
Aspen Global Congress on Scientific Thinking & Action: Vaccine Denialism: Death by Misinformation
March 19, 2021

I was invited by Aspen Congress Organizers to chair a panel discussion composed of paired interviews and small group discussions on “Vaccine Denialism: Death by Misinformation.” The aim of this panel was to examine current misinformation around the vaccine and how this impacts the response and control of the spread of the COVID-19 pandemic. Panelists Dr. Noel Brewer; Professor in the Department of Health Behavior at UNC; Ovidiu Covaciu; Science Communicator and Activist; Kavin Senapathy; Science Writer; and Fara Nydiaye; Deputy Executive Director for Speak up Africa shared their insights on trust in the public health system as well as how we can build trust in communities to deal with vaccine hesitancy.
Watch full video here: https://www.youtube.com/watch?v=ALaSceWRLyU&t=193s
CUGH 2021 Plenary Panel: African Leaders Addressing Critical Gaps in Global Health and Development
March 14, 2021

As part of The 2021 Consortium of Universities for Global Health (CUGH) virtual conference under theme “Addressing Critical Gaps in Global Health and Development, I moderated a panel discussion on African Leaders Addressing Critical Gaps in Global Health and Development. On this panel, I was joined by Dr. John Nkengasong, Director, Africa Centers for Disease Control and Prevention (CDC); Dr. Tlaleng Mofokeng; Special Rapporteur on the Right to Health at the United Nations Human Rights Council; and Dr. John Amuasi; Executive Director of the African Research Network for Neglected Tropical Diseases. Panelists discussed the importance of understanding our continent’s historical narrative and also investing in home-grown solutions focused on research. In this session, speakers highlighted some successes, challenges, as well as solutions that can be taken to promote development of African countries.
Watch full video here: https://cugh.confex.com/cugh/2021/meetingapp.cgi/Session/1325
CUGH 2021: Women Leaders in the COVID-19 Pandemic Response
March 13, 2021
As part of The 2021 Consortium of Universities for Global Health (CUGH) virtual conference under theme “Addressing Critical Gaps in Global Health and Development, I joined a great panel on women’s leadership hosted by Baylor College of Medicine. In my presentation titled: “Women in Global Health: Challenges and Triumphs,” I talked about how gender inequity plays a role in the representation of women leaders in academia, research, and the global public health response to this pandemic and share lessons we can learn to move forward. In my discussion, I provided examples of research that has shown when comparing countries led by men and those led by women, countries led by women responded better to the pandemic and were quick to implement evidence-based interventions which could be a reason for less COVID-19 related deaths. I share lessons from Rwanda where laws and policies promote gender equity across all sectors. Moreover, the University of Global Health Equity (UGHE) focus on ensuring female representation in the global health sector is another example of gender equity promotion.
Watch full video here: https://cugh.confex.com/cugh/2021/meetingapp.cgi/Session/1199
CUGH 2021: Exemplars in Global Health: Learning From Exemplars in Global Health: Mitigating the Indirect Effects of COVID-19 on Maternal and Child Health
March 13, 2021
As part of The 2021 Consortium of Universities for Global Health (CUGH) virtual conference under theme “Addressing Critical Gaps in Global Health and Development, I joined a panel of experts to discuss how how countries employed strategies for delivering interventions and structured programs to achieve health gains during past emergencies as well as present emerging findings on innovative strategies to maintain essential health services and mitigate the impact of COVID-19. In my presentation titled: “Rwanda Leveraged Strategies for reducing U5M to respond to COVID-19 and Maintain RMNCAAH Services During the Pandemic,” I share lessons on Rwanda’s unique strategic, implementation and monitoring plan to streamline all COVID-19 response activities. Rwanda also leveraged CHWs who played a role in training and sensitizing citizens to follow national prevention and management guidelines. Leaders across different sectors prioritized the vulnerable and ensured that support such as free testing, treatment services, food, and other supplies were distributed among those who could not afford to follow COVID-19 regulations. In response, the country also adopted innovative strategies such as digital data collection, use of robots and drones to support the COVID-19 response. In Rwanda, antenatal visits, health facility deliveries, and vaccinations were always maintained throughout the pandemic response.
Watch full video here: https://cugh.confex.com/cugh/2021/meetingapp.cgi/Session/1224
CUGH 2021: Transforming Research Results into Policies and Implementation Strategies
March 12, 2021
As part of The 2021 Consortium of Universities for Global Health (CUGH) virtual conference under theme “Addressing Critical Gaps in Global Health and Development.” I joined a session organized by the University of Global Health Equity on Transforming Research Results into Policies and Implementation Strategies. In my presentation titled: “Maintenance of Maternal and Child Health Services during COVID-19 Using Strategies for Under-five Mortality Reduction,” Using Rwanda as example, I talked about what the country did to maintain essential health services during the COVID-19 pandemic by using the implementation strategies that were used to reduce U5 mortality between 2000-2015. In response, Rwanda adopted key approaches including using a national and unique strategic plan, leveraging Community Health Workers (CHWs) by training them to sensitize their community members about COVID-19 prevention behavior, using data to inform policies, as well as adopting innovations. Through adopting these factors, Rwanda maintained the percentage of antenatal visits, health facility deliveries, and continued to vaccine children.
Watch full video here: https://cugh.confex.com/cugh/2021/meetingapp.cgi/Session/1206
National Cancer Institute, National Institutes of Health CUGH 2021 Satellite Session: Strategies to Address Global Health Inequities
March 8, 2021
As part of The 2021 Consortium of Universities for Global Health (CUGH) virtual conference under theme “Addressing Critical Gaps in Global Health and Development,” I was invited by Monica Webb Hooper from the National Institute on Minority Health and Health Disparities (NIMHD), Vidya Vedham from the National Cancer Institute (NCI) to participate in a CUGH satellite session on Strategies to Address Global Health Inequities. In my presentation titled: “Funders’ Responsibilities to Achieving Global Health Equity,” I talked about the contribution of funders in decolonizing global health and their responsibilities to implementing strategies and actions that are guided by equity. I started by discussing the economic context of countries in the Global South because of Western interference in their political, social, and family contexts. I also highlighted the role of aid as a tool that has continued to be used for neo-colonialism. In addition, I discussed the importance of funders taking responsibility and accountability to protect human right to health for all people but most of all focusing on the vulnerable. In this regard, taking the University of Global Health Equity (UGHE) as an example, we need to fund and fundraise for global health education that reinforces the ideals of equity and teaches students to recognize and address vulnerabilities. I called on the audience to not stay silence, everyone has a role to play. We all need to put respect, value, and real knowledge and skills at the heart of all finances and requests for funding without leaving anyone behind.
Watch full video here: https://cugh.confex.com/cugh/2021/meetingapp.cgi/Session/1271
The Wharton School- University of Pennsylvania: The Transformative Power of Women’s Leadership: Lessons from Rwanda
March 8, 2021

To observe International Women’s Day, I was invited by the Wharton School at the University of Pennsylvania to participate in a panel discussion on “The Transformative Power of Women’s Leadership: Lessons from Rwanda.” In this session, I spoke alongside fellow Rwandan women leaders, Dr. Diane Karusisi, CEO, Bank of Kigali, and Kampeta Sayinzoga, CEO, Development Bank of Rwanda Plc. The session was opened by Erika James, Dean of the Wharton School, Wharton and moderated by Professor Katherine Klein. I shared my experience as a female leader in Rwanda and most of all the critical role of the gender equity agenda in Rwanda’s progress and development. In Rwanda, the population trusts in the health sector and government and this trust is crucial to any progress the country has achieved across all sectors. For this equity agenda to work, Rwanda adapted laws, strategies, and action plans to ensure that women were part of Rwanda’s development plan and economic journey.
To learn more: https://alumni.wharton.upenn.edu/event/the-transformative-power-of-womens-leadership-lessons-from-rwanda/
The 3rd Annual Harvard Undergraduate UNICEF Club Conference Empowering Humanity
February 29, 2021

On February 29, I was invited by the Harvard Undergraduate UNICEF Club to speak in their Empowering Humanity conference to discuss the role of evidence-based governance in responding to COVID-19 and the health needs of children. In my presentation titled: “Empowering Humanity: Goals, Governments, and Growth: What Good Governance Meets for Children and Their Future,” I showed how Rwanda leveraged the same implementation strategies used to reduce under-five mortality between 2000 and 2015 to respond to COVID-19 and maintain existing essential health services. By controlling the pandemic effectively through evidence-based governance and the implementation of known interventions, we are preparing the country to return to a state of normalcy sooner. This allows children to resume their normal activities such as schools and access to mental health services, thereby maintaining their mental, emotional and social wellbeing.
To learn more: https://www.harvardunicef.org/conference
British Columbia Quality Forum 2021 Virtual Conference
February 26, 2021

In this session, I joined the British Columbia Patient Safety & Quality Council 2021 conference to share how Rwanda built a quality healthcare system, and how this strengthened healthcare system was built on equity and trust. During this keynote address titled: “Building a Quality Healthcare System: The Rwandan Experience,” I used the reduced Under 5 Mortality rate as an indicator of the progress in healthcare delivery, and enforced the idea that the problem is the system and not the individual, exploring the idea that systems must start with effective, quality provision of services to underserved populations using equitable frameworks. I shared with the audience that in Rwanda, we focus on creating and strengthening systems that leave no one out and most especially the vulnerable. This is because we know that when the vulnerable are served, we are all served.
Watch full video here: https://www.youtube.com/watch?v=NJdObLnScQg
#AskProfAgnes webinar series: Overlooked Injustices Faced by Persons Living with Disabilities During COVID-19 and Beyond
February 22, 2021

As a continuum of the monthly global debate on social, #AskProfAgnes and on the occasion of the UN world Day of Social Justice, I invited a panel of prominent leaders and experts from diverse backgrounds discussed the overlooked injustices to explore the overlooked injustices persons with disabilities face before and during this current pandemic as well as discuss solutions. I chaired this panel and it hosted by Dr. Zahirah McNatt, Assistant Professor and Godley-St. Goar Chair of the Department of Community Health and Social Medicine, UGHE. Mr. Maxwell Gomera, Maxwell, UNDP representative in Rwanda shared with us the global situation of persons living with disabilities and the UN recommendations on legal and policy frameworks that provide protection to Persons with Disabilities during COVID-19. Our second panelist, Dr. Cheri Blauwet Assistant Professor of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Network, Harvard Medical School (USA) discussed the data on the situation of disability in the U.S. and the consequences of COVID, exploring the professional inclusions of Persons with Disabilities in the U.S.A. Claudine Humure, Partnership Coordinator, UGHE & member of the Rwanda Society of Prosthetists and Orthotists (Rwanda) talked about the data on the situation of disability in Rwanda, the national legal and institutional protections, and what was done in Rwanda to mitigate disadvantages linked to disability during the COVID-19 period. Rupsa Mallik, Director of Programs and Innovation, Creating Resources for Empowerment in Action (India) joined us from India and shared the situation of Persons living with Disabilities in South Asia, and the role of NGOs to leverage resources and solutions for people with disabilities during the pandemic.
Watch full video here: https://www.youtube.com/watch?v=-SpwevCbDV4
OneDartmouth Lecture Vaccine Series: Eye on Equity: COVID-19 Vaccine Distribution in the U.S and Worldwide
February 21, 2021
At the invitation of Amanda J. Bassett, Director of Alumni relations, I served on a panel titled “Eye on Equity: COVID-19 Vaccine Distribution in the U.S and Worldwide” for the Dartmouth College Geisel School of Medicine moderated by Susan Dentzer, Senior Policy Fellow, Robert J. Margolis Center for Health Policy Duke University. On this panel, I discussed Rwanda’s response to healthcare delivery during COVID-19 and how its healthcare system has worked hard to achieve equitable access to care and services. I used lessons from HPV vaccination rollout and antiretroviral therapy rollout as examples where she solidified to the audience the fact that equity in access to life saving techniques is the only way forward for global health for all. I also highlighted that regional collaboration during COVID-19 became a responsibility, and equitable quality procurement required this action to ensure proper supply of the vaccine.
Watch full video here: https://www.youtube.com/watch?v=jxOfw1Rwr34
13th Annual Renee C. Fox Lecture University of Pennsylvania Perelman School of Medicine
February 19, 2021

On February 19th, I was invited by Dr. Michael Parmacek to serve as the 13th annual Renee C. Fox Lecturer in Medicine, Culture, and Society which is part of the University of Pennsylvania’s Perelman School of Medicine Distinguished Medical Grand Rounds Speaker Series. This lecture was established to honor Dr. Renee C. Fox. Under the title “What went wrong and What went well in the World: Lessons on COVID management”, I discussed how poor global COVID-19 predictions exemplified colonialism and Western bias that is detrimental to the world, as well as the role of equity as a core element of effective leadership and resilient health systems building. I called on the audience to learn from Rwanda’s successful response to the pandemic which lies in part to its adoption of the multi-sectoral approach. In Rwanda, we understood that the pandemic not only affects the health sector, but also the economic, education, gender, and all other sectors.
Watch full video here: https://mediasite.med.upenn.edu/mediasite/Play/b61f8070f42c433db7064a8a7c7e440a1d
University of Michigan Africa Week: Distributing the COVID-19 Vaccine in Africa: Challenges and Opportunities for Collaboration
February 18, 2021
I was invited by Dr. Joseph C. Kolars, Director, UM Center for Global Health Equity to participate in University of Michigan-Africa Week. Alongside my colleague Dr. Paul Famer, Dr. Tachi Yamada facilitated an engaging and fruitful discussion around some of the challenges to COVID19 vaccine distribution on the African continent. In this discussion, I highlighted the importance of equitable vaccine distribution to ensure that Africa and other developing nations are not left behind. We discussed some of the challenges in vaccine access and distribution including parallel bilateral deals and hoarding vaccines by rich countries. However, I reminded the audience that we must ensure that the history of leaving developing countries behind when it comes to access to treatment should not repeat itself. Countries must come together to reaffirm their commitment to initiatives such as COVAX to ensure that low-incomes countries take part in vaccinating their populations without delays.
Watch full video here: https://www.youtube.com/watch?v=wZnGJo_fsp
17th National Health Summit 2021
February 10, 2021

On February 10, I delivered a keynote address at the 17th National Health Summit under the theme Future-proofing our health system for a post-Covid world. This summit is Ireland’s longest running healthcare management conference. In my presentation titled: “A Formula for Health Equity: The moral imperative to build an equity-based health sector prepared to respond to health threats,” I discussed the factors that are key to building an equitable healthcare system that provides quality services to all and is prepared to respond to health crises such as the COVID-19 pandemic using examples from Rwanda. I shared eight key factors that guide Rwanda’s health equity agenda. First, accountability to our true bosses who are the communities that we serve. Second, a clear equity agenda and ensuring that it is embedded into policy, strategies, and guidelines. Third, provision of quality health services and ensuring collaboration across all sectors and community participation as well. Moreover, we live in an interconnected world and have a moral obligation to global solidarity. We also need to cultivate quality research and build resources for data sharing to ensure improvement functionality in the implementation of evidence-based interventions for the vulnerable, & train clinicians in leadership with cultural humility to listen. To achieve health equity, we finally need to invest in training the next generation of global health leaders and this is what we are doing at the University of Global Health Equity.
Watch full video here: https://drive.google.com/drive/u/1/search?q=ireland%20health%20summit
Duke Global Health Institute, the Samuel DuBois Cook Center on Social Justice, and the Duke Department of Cultural Anthropology present “Epidemic Illusions: On the Coloniality of Global Public Health: A Book Talk with Eugene Richardson”
February 8, 2021
On February 8, I participated on a panel session organized by the Duke Global Health Institute, the Samuel DuBois Cook Center on Social Justice, and the Duke Department of Cultural Anthropology at Duke University. I was invited by Dr. Kearsley (Karrie) A. Stewart, Professor of the Practice, Global Health and Cultural Anthropology at Duke University. On this panel, Dr. Eugene Richardson discussed his new book Epidemic Illusions: On the Coloniality of Global Public Health in conversation with myself, Dr. Paul Farmer and Dr. William Darity Jr. I was invited to talk about the link between the hypothesis and demonstration of the book to the role of the University of Global Health Equity (UGHE) as an institution dedicated to health equity. This book is very important as it encapsulates the core problems in global health today. In my presentation titled: “UGHE: A Model African Institution Decolonizing Global Health and Challenging Inequities”, I discussed how UGHE is decolonizing global health education by training our students to question existing health systems and humanitarian misconduct without leaving anyone behind especially the vulnerable. I shared key points on how global health education is inaccessible to participants from low-income countries due to cost and location. However, at UGHE, we provide a medical education for many on the African continent who cannot afford their education. We bring together future global health leaders who look beyond the exam room to fully understand the social determinants of health and respond to disparities.
Watch full video here: https://www.youtube.com/watch?v=0xttpHnEQ9g&t=3s
Centre for International Child Health 3rd Annual Conference: Global Child Health, Beyond the Pandemic
January 28, 2021

On January 28, I joined the Centre for International Child Health (CICH) at British Columbia’s Children’s and Women’s Hospital in Canada as a keynote speaker to discuss the impact of the COVID-19 pandemic on children. While the pandemic presents a lower direct risk of illness for children, it significantly impacts their mental health, social and economic wellbeing, as well as their progress in their educational achievements. Through my presentation titled, “Reimagining Global Health Education to Support Children during Health Crises”, I highlighted the importance of addressing the various social determinants of health to ensure that children are protected during health crises. I gave various examples of the non-physical impacts of the pandemic of children such as the increase in mental health difficulties, disruption of key child health services such as vaccinations, increase in their exposure to violence as well as the interruption of their education. We can only address these challenges if our medical and global health education systems teach our students to pay attention to all the different aspects of health – not just the physical. This is what we are doing at the University of Global Health Equity through an education system that takes a biosocial approach, makes community engagement at the center of all educational activities, and teaches leadership and management skills to ensure that our students are capable of leading equitable healthcare systems.
Watch full video here: https://vimeo.com/510013076
Core Group Global Health Practitioner Conference
January 28, 2021
On January 28, I joined the 2021 CORE Group Global Health Practitioner Conference. Under the theme prioritizing child and adolescent health in the upcoming decade, the Exemplars session focused on strategies for maintaining child health services during the COVID pandemic, drawing lessons from Rwanda and Bangladesh. During the session titled “Unlocking Potential: Prioritizing Child and Adolescent Health and Well-Being in the New Decade,” I gave a presentation on “Lessons for Maintaining Essential Child Health Services During the COVID-19 Pandemic from the Rwandan Context.” In this presentation, I discussed how Rwanda used several implementation strategies to reduce under-five mortality between 2000 and 2015. I shared with the audience strategies that the country leveraged to respond to the COVID-19 pandemic and to reduce its indirect impact on the availability and usage of child health services and gave examples on how this was accomplished. Lessons from Rwanda to maintain child health services include commitment to equality, consistent communication, innovation in technology, and an emphasis on using data and evidence.
Learn more: https://coregroup.org/event/core-group-2020-global-health-practitioner-conference-ghpc/
UNESCO Expert Group on Universities 2030 and University of Bergen
January 25, 2021
I serve as one of fifteen experts on Universities invited by UNESCO to help support the writing of a report that proposes guidelines and actions for how universities can facilitate knowledge development as well as new research and education strategies that can generate the deep-going social, economic and environmental transformations needed. Sustainable Development is a concerning issue during these unprecedented times, and the final output of collective knowledge on this pressing issue will be a great resource. This report will push to ensure equity in disciplines, gender, and geographical location and is working well on strengthening social, economic, and environmental changes needed for a sustainable future in higher education.
Learn more: https://www.uib.no/en/sdgbergen/141190/unesco-global-independent-expert-group
Dartmouth Geisel School of Medicine: 15th Annual Geisel Martin Luther King Jr. Health Equity Celebration
January 18, 2021

On Martin Luther King Jr Day, I joined future medical health professionals at the Geisel School of Medicine at Dartmouth College in the USA to discuss the legacy of MLK and bring awareness to inequalities in health. I gave a presentation titled “More than ever: “Of all the forms of inequality, injustice in health is the most shocking and the most inhumane” Dr. Martin Luther King Jr. I spoke about how poor health outcomes across diverse minority groups are due to the social determinants of health and these are the economic and social conditions or non-medical factors that influence individual and group health outcomes. In my presentation, I highlighted that these social determinants of health affect minority communities at a disproportionate rate, especially Black Americans. As I examined the way forward, I reminded future health professionals to not stay silent. What about the next crisis? To prepare for any future global health threat, we need governance structures centered on wellness and inclusiveness. “We need to listen to minorities through humility, focus on truth and cultivating trust with patients of different communities and above all respect, value and love each person around you for the human they represent.”
Learn more: https://geiselmed.dartmouth.edu/dice/mlk/
8-week course: Introduction to Global Health
January 16, 2021

For eight weeks until the 27th February, UGHE is partnering with Socios En Salud and other partners on a free 2 month course delivered virtually in both English and Spanish – giving participants an Introduction to Global Health. This is an 8 week course with 2 sessions per week: theory & case study discussion. I participated in Session 2 covering “Global Health Inequities & Structural Violence: How Critical Race Theory and Post-Colonial Theory Can Guide Us”. I gave a brief update on Partners in Health Rwanda/Inshuti Mu Buzima (IMB) and UGHE, and their successes, challenges, and impacts, and discussed the effects of COVID on education programs. Registrants of this course learned and understood how and why racism and colonialism are pervasive systems that shape how we think. I also explored how critical race theory and post-colonial theory can serve as tools for health equity and health care delivery and challenge current thinking and paradigms which separate and silo structural change and health care. Additionally, I talked about the modern context of these inequities in the countries of Peru, Haiti, and Rwanda and the need for inclusive access as a global concern using examples of how Rwanda achieved development through an equity lens. The pandemic has exacerbated this issue, and I stressed the need to find innovative ways to continue education at all levels and reimagine education, using COVID-19 responses lessons.
Learn more: https://sociosensalud.org.pe/
Project Syndicate and the Center for International Media Assistance Present “The World in 2020:Redefined” at the Occasion of UNESCO: World Press Conference 2020
December 10, 2020
On December 10, 2020, I joined an opening panel for UNESCO’s World Press Freedom Day celebration. The panel titled “The World in 2020: Journalism Redefined” was organized by Project Syndicate and the Center for International Media Assistance. The panel focused on defining issues in 2020, namely, the COVID-19 pandemic and elections/protests and global movements and their impact on the media. I shared about how there has been different levels of performance of the media in covering the pandemic; some relying on science to present factual information about the pandemic and others have been impacted by political groups to present inaccurate information. “The failure of the media in providing accurate information about the pandemic results in the decrease of trust that is very crucial when responding to any health threats. Communities will not abide”
Watch full video here: https://www.youtube.com/watch?v=r3g7TBbG2GE&t=970s
FIGO’s Africa regional congress: Challenging the Status Quo to Achieve Greatness as Women in Global Health Leadership
December 15, 2020

On December 15th, I joined FIGO’s Africa regional congress to give a keynote address on how we can challenge the Status Quo to Achieve Greatness as Women in Global Health Leadership. Through my presentation titled: “Challenging the Status Quo to Achieve Greatness as Women in Global Health Leadership,” I examined the gender disparities in academia, research, and global health leadership as well as provided guidance and examples on how we can challenge the status quo to advocate for and promote more women into leadership positions. I gave examples of the status of women in leadership whereby in the corporate world in Africa, among the top 307 African companies in 2015, women accounted for only 14% of total board membership. This means that there is one woman out of every seven board members and that one-third of the boards have no women at all. In healthcare, women make up majority of the global workforce but only hold 25% of leadership positions. Moreover, in Obstetrics and Gynecology, women face challenges seeking care due to lack of knowledge, transportation, and community awareness. Taking lessons from Rwanda, in order to make change, we need to improve status and opportunities for women, implement laws and policies through a gender equity lens, and as well as include gender budgeting across all sectors. To make global health representative “We need Collective Action for Institutional Change.”
Watch the full video here: https://drive.google.com/file/d/1oC1JuD94IdUJNsFmx80BuOgsKgZn4t9a/view?usp=sharing
NEF Global Gathering: “The role of science in informing recovery from a global crisis such as COVID-19”
December 8, 2020

Under the theme “Building Africa’s resilience through education, research and innovation.” for the online New Einstein’s Forum-Global Gathering 2020, I joined a diverse panel of to discuss “The role of science in informing recovery from global crises such as COVID-19”. We shared our expertise in science’s role in informing policy and society in the response to COVID-19 and ensuring the successful implementation of the designed policies in African countries and across the world. I also shared about the role of young African scientists in supporting the continent to implement the right policies based on scientific facts. Young African scientists need to have self-esteem and confidence in the work that they do on the continent and beyond. However, we are all responsible as Africans to foster an environment that supports development of the research field to build research capacity on the continent.
Watch full video here: https://www.facebook.com/577158062337590/videos/3128144730624067
University of Global Health Equity and Imperial London College Present a Virtual Conference on “Transforming Amputation and Prosthetic Services Globally”
December 5, 2020

It was my pleasure to welcome attendees to the virtual conference on Transforming Amputation and Prosthetic Services Globally, jointly hosted and delivered by the University of Global Health Equity (UGHE) and Imperial College London. The conference aimed to address, and encourage discussion around the key areas of the amputee service pathway. “Together, we must work to make the world more inclusive for the more than one billion people living with a disability. Our value at UGHE to leave no one behind means that we must ensure amputees in our communities are listened to and given a seat at the decision-making table. There is a need for community recognition of amputee identity and a commitment to transform the way we care for persons with disabilities.”
Watch full video here: https://www.youtube.com/watch?v=UEqc_PVh73s&feature=youtu.be
The University of Ottawa Faculty of Medicine 75th Anniversary International Collaboration Webinar Series: “Achieving Health Equity: A Conversation with the Vice Chancellor of the University of Global Health Equity in Rwanda“
November 27, 2020

I joined Sanni Yaya, Professor of Economics and Global Health, Director and Associate Dean of the School of International Development and Global Studies, University of Ottawa in Canada in an interview as part of the Faculty of Medicine 75th Anniversary International Collaboration Webinar Series. We discussed key advancements made to Rwanda’s health care system in the past 20 years such as improvements in the economic sector also contributed to improvements in the health sector and Rwanda’s development of the community health insurance program through which individuals pay according to their income level. I shared about the role UGHE in addressing social determinants of health. Our students are taught that medicine is beyond the physical manifestations of the disease and they work in the communities that they will serve in the future.
Watch full video here: https://www.youtube.com/watch?v=UAUWitCnlMY&feature=youtu.be
Inaugural International COVID-19 Data Alliance Forum
November 19, 2020

In July 2020, the International COVID-19 Data Alliance (ICODA) was launched with the mission of producing a safe global platform for data access, use and analysis that respects confidentiality. As Co-Chair of the of the International COVID-19 Data Research Alliance, Science & Strategic Advisory Council, I joined my colleagues to give opening remarks for the Inaugural ICODA Forum. This platform allows researchers from all over the world to collaborate, share, and access global data in a secure way to derive insights about COVID-19. To rapidly find a global solution in the fight against the COVID-19 pandemic, we need to share our capacity, knowledge, and expertise between continents, countries, experts, researchers, clinicians, and communities.
Watch full video here: https://www.youtube.com/watch?v=0KqEi3b9UXk
U.S. Global Leadership Coalition: Mid-Atlantic Regional Summit
November 16, 2020

In the backdrop of COVID-19, I joined Senator Chris Coons and esteemed leaders for the Mid-Atlantic Regional Summit, virtual town hall on the positive impact of global affairs in the Mid-Atlantic Region. I shared about our work at the University of Global Health Equity (UGHE) focusing on delivering quality and equitable health care for all. I also discussed the importance of vaccine distribution around the world in order to fight the COVID-19 pandemic. If there is no fair distribution of the COVID-19 vaccine and all vaccines, we will not as a planet be rid of this pandemic on time. The world needs to come together in solidary and no country will be safe if one country is not safe.
Watch full video here: https://www.facebook.com/watch/live/?v=364433121529836&ref=watch_permalink
Behind the Scenes of Bending the Arc: Celebrating the Film & its Message through the Lens of its stars
October 27, 2020

This October, the highly-acclaimed documentary Bending the Arc was released on Netflix, intriguing audiences globally with its gripping narrative chronicling real-world heroes at the center of some of the world’s most pressing humanitarian crises. I had the honor to join my friends and colleagues PIH co-founders Dr. Jim Yong Kim, Ophelia Dahl, and Dr. Paul Farmer; PIH Chief Medical Officer Dr. Joia Mukherjee; and UGHE Co-Founder & Member of the Vice Chancellor’s Advisory Board Dr. Peter Drobac to discuss our friendship as the golden thread to our equity agenda. In this discussion, I made the link between what we see in Bending the Arc and what Rwanda is doing to fight COVID-19. As seen in the documentary, Rwanda has learned to use evidence-based interventions when tacking problems. In Rwanda, we strived to build a health sector system based on equity that leaves no one out. Community Health Workers play a big role in the community and we have built on that trust in the community to fight against COVID-19 in the country. I want to encourage everyone to watch the documentary because it is needed today and it will be needed tomorrow because COVID-19 will not be the last pandemic but the vulnerable and marginalized will always be left out and systems that will work are those based on equity and inclusivity.
Watch full video here: https://www.youtube.com/watch?v=JMVqFmZuFMI&feature=youtu.be
The Commonwealth Action Series: “Fighting The Biggest Killer Of Youth In The Commonwealth”
October 27, 2020

As part of the Commonwealth Action Series, I kicked off the session “Road crashes as a public health threat” to provide an overview of the burden of road injury in the commonwealth. Road injuries are the leading worldwide cause of death for children and young people aged 5-29 years. I discussed the importance of recognizing the implications of road safety through an equity, economic, and accessibility lens especially for the youth. We need a multisectoral coordinator to bring sustainable economic and legislature effects to prevent road traffic injuries. Moreover, policies need to make road safety part of the wider agenda for achieving Sustainable Development Goals.
Watch full video here: https://www.facebook.com/claimingourspace/videos/353195102453814/
WLGH Conference 2020: Succeeding as a Woman in Academia: Battling a Pandemic and the Patriarchy
October 15, 2020

The Women Lift Health Organization in partnership with the Stanford Center for Innovation in Global Health, led the Virtual 2020 Women Leaders in Global Health 2020 Conference that lasted from October 13-15th. Under the theme, commit, connect, act, diverse women came together to discuss the collective vision for global health. This conference gave the opportunity for women, and men, across sectors, disciplines and continents to share ideas and information about women’s leadership in health. On the last day of the conference, I was a panelist alongside Dr. Michele Barry, founder of WomenLift Health, Prof. Heidi Larson, Director of The Vaccine Confidence, and Dr. Gagandeep Kang, Professor at the Wellcome Trust Research Laboratory. We participated in a global dialogue under the theme, Succeeding as a woman in academia: Battling Pandemic and Patriarchy. The discussion for this breakout panel session surrounded how we can leverage women scientists and researchers who are underrepresented in academia.
Watch full video here: https://www.youtube.com/watch?v=3x4qwi7R9yU&feature=emb_title
University of Global Health Equity presents a webinar on “Child and Adolescent Mental Health: Mental Health in the Time of COVID-19 in Rwanda and Beyond”
October 15, 2020
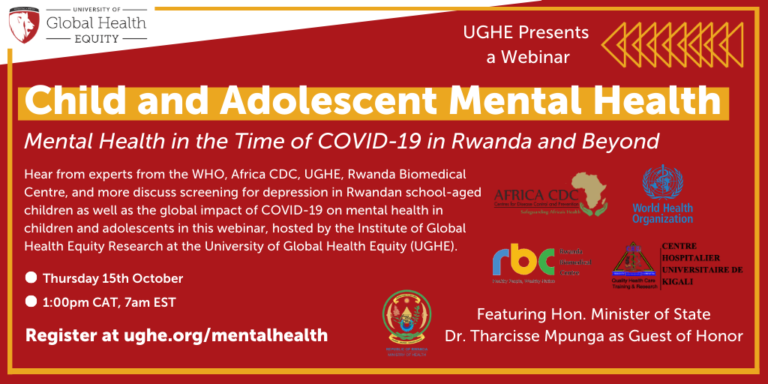
Every year the World Health Organization observes World Mental Health Day in the month of October. To mark this occasion, the Institute of Global Health Equity Research (IGHER) at the University of Global Health Equity (UGHE) hosted an event to discuss child and adolescent mental health under the patronage of the Honorable Dr. Tharcisse Mpunga, the Minister of State in the Ministry of Health and Two keynote speakers from WHO and Africa CDC. In the first session, I and experts from the Rwanda Biomedical Center presented on the development and validation of the Child Depression Screening Tool (CDST), a rapid, easy-to-use, open-source tool used to screen the risk of depression among children. The CDST will be used in to screen child at risk of depression in schools. In the second session, panelists hailing from Africa, Oceania, and USA, shared valuable lessons learned around children and adolescent mental health and the impact of the COVID-19 pandemic through the lens of different contexts.
Watch the full video here: https://www.youtube.com/watch?v=8QICJMTv7OA&feature=youtu.be
University of Global Health Equity Hosts a Webinar on “World Patient Safety Day: Health Worker Safety in a Time of Pandemics”
September 17, 2020
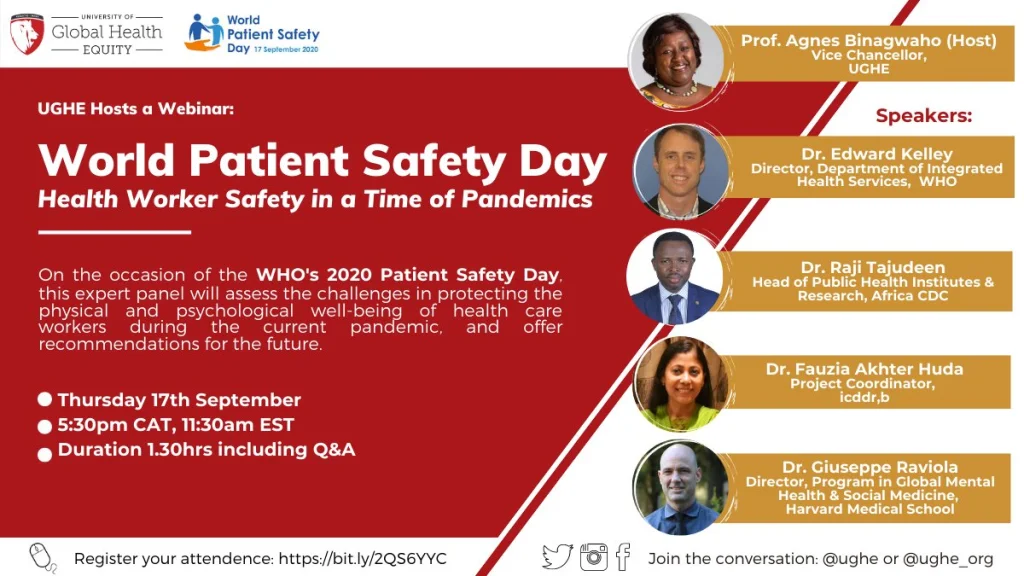
I had the privilege to host a UGHE webinar to mark the occasion of WHO’s World Patient Safety Day. Joined by a great panel of experts, we discussed how healthcare worker safety is integral to patient safety, and identified and assessed both the challenges in protecting the physical safety and mental health of health care workers in the current pandemic, as well as their access to needed resources (including PPE and psychological counselling). Panelists included Dr. Edward Talbott Kelley, PhD, Director, Department of Integrated Health Services, World Health Organization; Dr. Raji Tajudeen MD, MPH, FWACP, Head of Public Health Institutes & Research, Africa CDC; Dr. Fauzia Akhter Huda, Project Coordinator, icddr,b; and Dr. Giuseppe Raviola, MD, MPH, Director, Program in Global Mental Health & Social Medicine, Harvard Medical School. As we continue to fight against the COVID-19 pandemic, it is important to continue recognizing the work of health workers around the world. We thank all the healthcare workers for their commitment to caring for their communities.
Watch full video here: https://www.youtube.com/watch?v=0RgJhzIUaDw
Stanford King Center for Development at Stanford University presents “COVID-19: The Impact in Africa”
September 16, 2020
I was honored to join Belinda Archibong, assistant professor of economics at Barnard College, Columbia Universityand Albert G. Zeufack, the World Bank’s chief economist for Africa for a discussion on the impact of COVID-19 in Africa hosted by Stanford’s King Center for Development. On this panel, I examined the impacts of COVID-19 on health outcomes and health systems in Sub-Saharan Africa compare to US and Europe and the contributors to the pandemic response. I shared about the Western Supremacy Mentality, the expectation that Africa would fail to respond to COVID-19. The Global Health Security index predicted that the US was the most prepared country, but we have seen otherwise. Taking lessons from Rwanda, we used Evidence-Based Interventions to respond to the pandemic. This was done by using data and following science to implement policies and guidelines.
Watch full video here: https://www.youtube.com/watch?v=WLh5tYEGBXs&feature=youtu.be
NCDI Poverty Network Hosts NCDI Poverty launch-NCDIs and Poverty: How Do We Change Business as Usual?
September 15, 2020

As part of the global NCDI Poverty launch, I moderated a penal discussion on NCDIs and Poverty: How Do We Change Business as Usual? The speakers inlcuded Sania Nishtar, Special Assistant on Poverty Alleviation and Social Safety, Pakistan;Matshidiso Moeti, Regional Director, WHO AFRO; and Lea Kilenga, Executive Director of the Africa Sickle Cell Organization. This was a very interesting, conversation through which we deeply explored solutions to finance, advocacy, and the strengthening of the capacity of health systems.
Watch full video here: https://www.youtube.com/watch?v=R4IZ_R11MKU
RIGHT TO HEALTH ACTION: “Country- & Community-Led Responses: Creating Sustainable Solutions to a Global Pandemic”
August 29, 2020
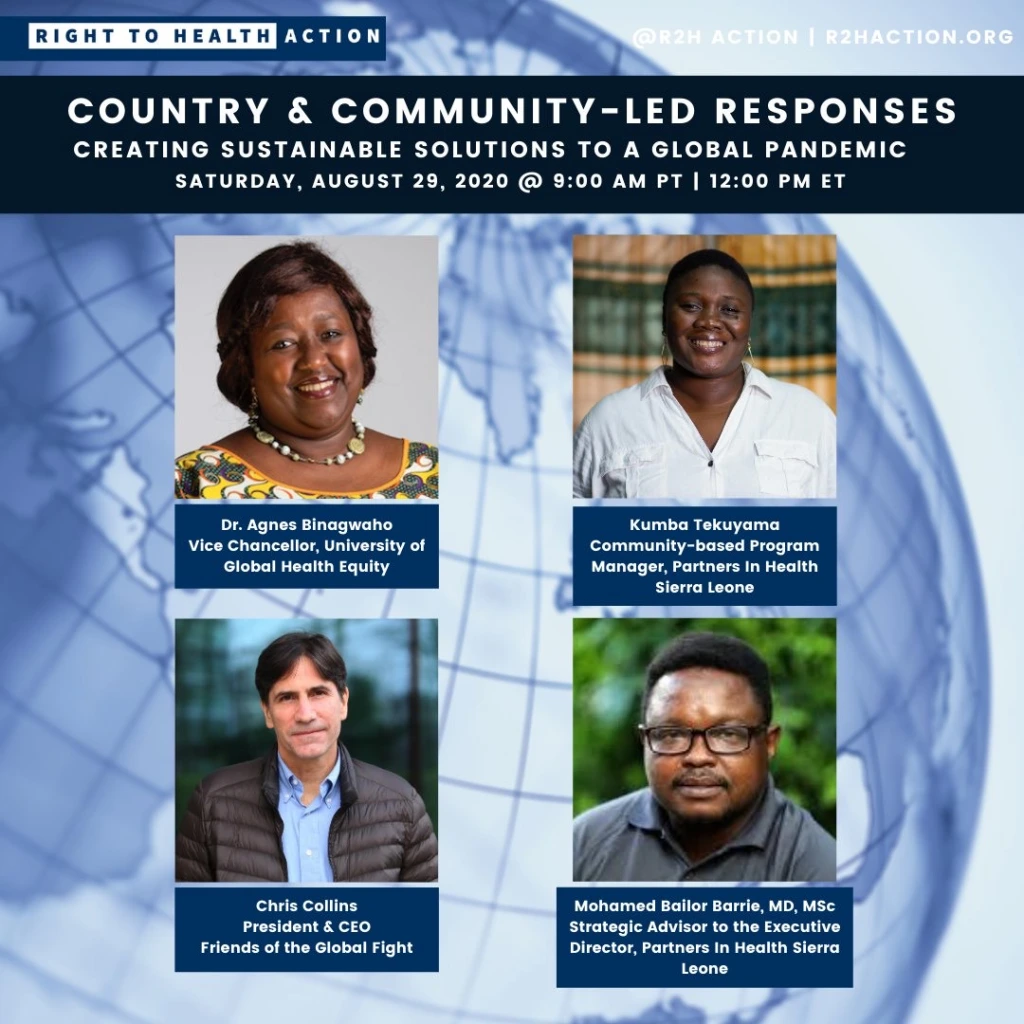
The current COVID-19 pandemic has disrupted families, communities, and countries around the world. Joined by great leaders, I had the privilege of participating in RIGHT TO HEALTH ACTION’s panel discussion on creating sustainable solutions to a global pandemic like COVID-19. I was joined by Chris Collins, President and CEO at Friends of the Global Fight Against AIDS, Tuberculosis and Malaria; Kumba Tekuyama, Community-based Program Manager, Partners In Health Sierra Leone; and Dr. Bailor Barrie, Strategic Advisor to the Executive Director, Partners In Health Sierra Leone. We know that we will face more pandemics in the future, and it is our duty to prepare for it.
Watch the full video here: https://www.youtube.com/watch?v=1LxPjYLMgHE
Rush University: Presidential Lecture Series
August 3, 2020

I had the opportunity to virtually speak at Rush University’s Presidential Lectures Series to discuss the “Moral Imperative to Build an Equity-based Health Sector Prepared to Respond to Health Threats.” I spoke about Rwanda’s response to COVID-19 and the importance of evidence-based decisions to keep the country’s COVID-19 spread under control. In the fight against COVID-19, accountability is key. This helps fight corruption and improves human development, with a focus on the most vulnerable. I also reminded the audience that Trust is a social determinant of health. In order to protect communities against COVID-19, people must understand that you are trying to protect them.
Watch the full video here: https://www.youtube.com/watch?v=9pPArUFBxZ
The University of Global Health Equity Hosts a webinar on “Implementation Science-Why It’s Needed Now, More than Ever”
July 21, 2020

I had the opportunity to join the University of Global Health Equity’s panel to discuss the significant role of implementation science during COVID-19 and future outbreaks. On the panel, I was joined by Dr. Lisa Hirschhorn, Professor of Medical Social Sciences & Psychiatry and Behavioral Sciences, Northwestern University; Dr. Quinhas Fernandes, Ministry of Health, Mozambique (Senior Public health staff), Implementation sciences program (Dep. Global Health), University of Washington; and Prof. Kenneth Sherr, Professor, Global Health, Adjunct Professor, Epidemiology, Adjunct Professor, Industrial and Systems Engineering. I shared about the need to increase the capacity to do research using implementation science. We always do not need to invest in new tools, we just need to use and maximize what we have and we will save millions of lives.
Watch the full video here: https://www.youtube.com/watch?v=TtT8oT7tf3w
Devex: On the Frontlines: A Conversation With Global Health Leaders
July 21, 2020
In the era of COVID-19, health workers are experiencing different challenges while on the front line of the fight against the pandemic. I was invited to join Devex in a timely panel discussion focused on amplifying calls for increased investment in capacity building for the healthcare workforce. On the panel, I was joined by Dr. Emanuele Capobianco, Director of Health and Care, IFRC; and Dr. Mickey Chopra, Lead Health Specialist, World Bank Group.
Watch full video here: https://www.youtube.com/watch?v=y-GlTClUdzM&t=384s
University of Aberdeen presents Evidence and Policy: What does follow the science really mean?
July 6, 2020
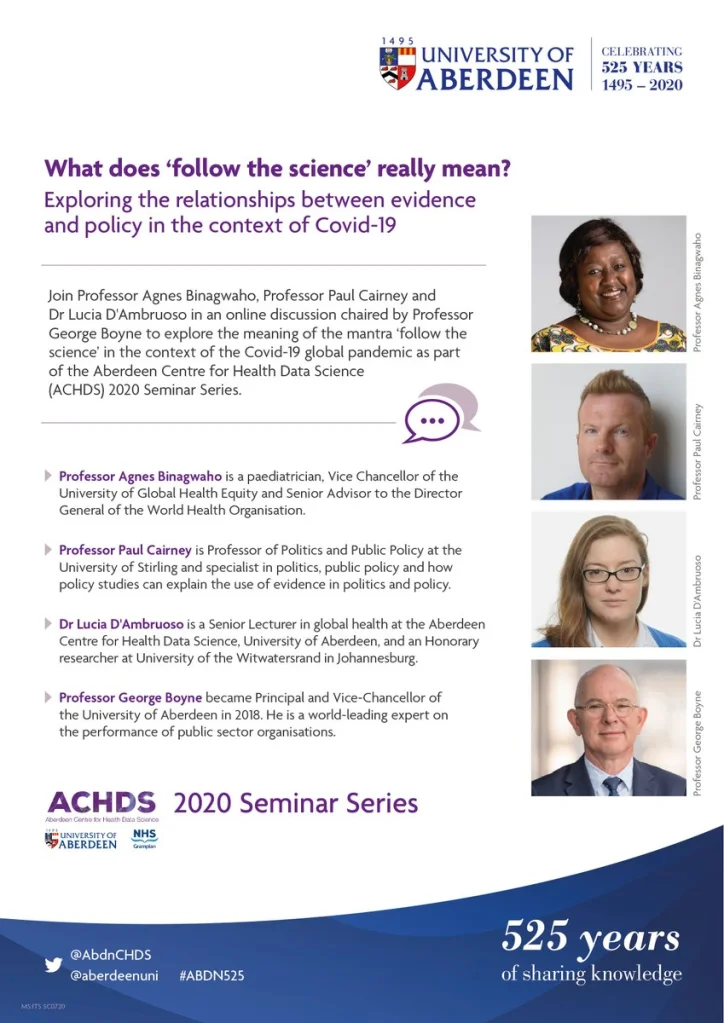
I had the honor to participate in a panel discussion hosted by the University of Aberdeen. The event was a discussion that explored the meaning of the mantra ‘follow the science’ in public policy responding to Covid-19, and looked at evidence-based policy making from the global south and north, as well as the role Universities have to support new ways to be inclusive, values-based evidence and accountability in public policy. The discussion was moderated by Professor George Boyne, Principal and Vice-Chancellor of the University of Aberdeen and panelists as a discussion between myself, Dr Lucia D’Ambruosom, Professor Paul Cairney an internationally renowned political scientist at Stirling University.
Watch full video here: https://www.youtube.com/watch?v=4oqa1bqJBOY&t=163s
WOW Global 24: Snapshots of Health and Hope
June 27, 2020

I had the honor to take part in the WOW: Women of the World Festival. The WOW Foundation is a charity that believes a gender equal world is desirable, possible and urgently required. The discussion focused on understanding what women’s sexual, physical, and mental health looks like right now. On the panel, I was joined by the chair, Jude Kelly, Founder and Director of The WOW Foundation (UK); Collie Mashaba, District Coordinator, (Mpumalanga, South Africa); Dr. Yasmeen Qazi, Family Planning & Reproductive Health Expert (Pakistan); Sonia Adesara, Medical Doctor (London, UK); and Madara Hettiarachchi, Director of Programmes and Accountability Disasters Emergency Committee (UK). As women at the forefront of global health responses, we looked at how the pandemic is affecting women, how we can protect women and girls, and what models can be used to get it right.
Watch full video here: https://www.youtube.com/watch?v=Yb3Qp2zBSuQ
Aspen Health For All: Leadership Lessons From Ebola to Fight COVID-19
June 3, 2020
On June 3rd, 2020, I had the opportunity to join Dr. Raj Panjabi, Co-Founder and CEO of Last Mile Health for a conversation hosted by the Aspen Global Innovators Group in which we shared our expertise on how African leaders can use lessons from Ebola to combat COVID-19. COVID-19 is a global crisis that needs everyone’s support, action, and intervention.
Watch the full conversation here: https://www.youtube.com/watch?v=cJkSpPZFmT8&feature=emb_title
CWL/CARE Virtual Health Forum
May 15, 2020

I was honored to take part in the CWL/CARE Virtual Health Forum, Connected Women Leaders, an initiative of the Rockefeller Foundation, which aims to connect women leaders across all sectors of life and work to activate networks in communities, and offer up ideas and solutions to address the world’s most urgent challenges. The lively discussion focused on COVID health care systems, and I offered my thoughts on Rwanda’s early preparation and capacity for emergency response, through national participation, information sharing, and a multisectoral approach. This important debate was moderated by Pat Mitchell, Co-Founder of Connected Women Leaders and Michelle Nunn, President & CEO of Care, and on the panel I was joined by Dr. Nana Twum Danso, Managing Director of Programs for Health at the Rockefeller Foundation, Prof Heidi J. Larson, Director of the Vaccine Confidence Project at London School of Hygiene and Tropical Medicine, and Ilhas Altinci, Sexual and Reproductive Health Advisor at Care, Turkey, Beth Cameron, Vice President, Global Biological Policy & Programs of the Nuclear Threat Initiative, and to close the session, Gayle E. Smith, resident & CEO of The One Campaign.
Read the transcript of my comments here: https://agnesbinagwaho.blog/2020/05/19/cwl-care-virtual-health-forum/
Watch the full video here: https://youtu.be/Zb98eh2GERk?t=953
McGill’s School of Population and Global Health: COVID-19 and the world’s vulnerable communities
April 30, 2020

I had the privilege to be invited to join McGill’s School of Population and Global Health in a timely panel discussion focused on how the most vulnerable in our global community have been and continue to be disproportionately affected by the COVID 19 pandemic. On the panel, I was joined by Dr. Ariel Pablos-Méndez, Professor of Medicine at Columbia University Medical Center; Patricio V. Marquez, former Lead Public Health Specialist, World Bank Group; Dr. Raj Panjabi, CEO of Last Mile Health; Dr. Joanne Liu, Associate Professor of Medicine at the University of Montreal and hosted by Dr. Timothy Evans, Inaugural Director and Associate Dean of the School of Population and Global Health, Faculty of Medicine, McGill, and Derek Cassoff, Managing Director, Communications, McGill Advancement. I spoke about the myth of “COVID 19 being a great equalizer” and about how the world needs to come together to support those among us who are most vulnerable.
Watch the full video here: https://mcgillnews.mcgill.ca/s/1762/news/interior.aspx?sid=1762&gid=2&pgid=2204
Per Fugelli Annual Lecture
December 12, 2019
I was honored to be the speaker at the 2019 Per Fugelli memorial lecture where I spoke about the journey of rebuilding the Rwandan health system in the wake of the 1994 genocide against the Tutsi. The principle of equity in health and dignity of the vulnerable is what lies at the center of Rwanda’s recovery based on solidarity and something that Dr. Fugelli spent his life fighting for. It was great to share Rwanda’s progress so far and reflect on how far we still have to go. The lecture was attended by members of the Rwandan diaspora in Norway, The Vice Dean and the student of Oslo University, and the family of the late Dr Fugelli.
Read more about the Per Fugelli lecture series here: https://www.med.uio.no/helsam/english/research/news-and-events/events/per-fugelli-lecture/
Commonwealth Road Safety Initiative
December 9-10, 2019

It was my pleasure to speak at the reconvening of the Commonwealth Road Safety Initiative hosted by the UK Department of Transport. As Co-Chair of the initiative, I gave a presentation titled “Putting Road Safety on the Commonwealth Agenda: A perspective from Africa”. I spoke about the emerging burden of road safety related deaths, especially in Africa, the example of some Rwandan campaigns to address these problems, and the way forward globally, with strong leadership, policies, a multisectoral approach to improve road safety. I look forward to continuing this conversation in future Commonwealth meetings, including CHOGM in June 2020 because road accidents remain the first killer of healthy young people under 30 around the world.
Read more about the Commonwealth Road Safety Initiative here: https://www.commonwealthrsi.org/
TEDWomen 2019
December 4, 2019

I had a lot of fun to being at the most recent TED Women event in Palm Springs, California where I joined impressive women leaders from around the world. My talk was about the strength I saw in Rwandan women prioritizing Rwanda’s recovery, development and forgiveness, and the significant impacts that occur worldwide when women are in leadership positions. I explained why we need more women in leadership roles, and that we need strong, educated African women to come back to Africa with their unique strength and contribute Africa’s development.
Read more about TED Women 2019 here: https://tedwomen2019.ted.com/
Watch the full TED talk here: https://www.ted.com/talks/agnes_binagwaho_how_women_are_revolutionizing_rwanda?utm_campaign=tedspread&utm_medium=referral&utm_source=tedcomshare
Tore Godal Honorary Lecture
November 23, 2019

I was honored to join my dear friend, Tore Godal, as he received the prestigious King’s Medal of Merit for his many decades of work in global health. The agenda of the ceremony consisted of lectures and panel discussions from global health actors on how far we have come and what the future of global health needs to look like. I had the privilege of presenting the keynote speech discussing what we should prioritize as we work towards achieving the SDGs emphasizing the need for smarter investment in building resilient health systems that can withstand future health threats.
Read more about Tore Godal’s career here: https://www.med.uio.no/helsam/english/research/centres/global-health/news-and-events/news/2019/report-dr.-tore-godal-awarded-with-the-king%E2%80%99s-meda.html
Hamwe Festival
November 8-13, 2019

From November 8th to November 13th, Artists, Creators and Global Health Leaders from across the world participated in the first edition of the annual Hamwe Festival, created by UGHE to celebrate the collaboration between the health sector and the creative industries. These two fields can and have historically worked together to bolster the global health agenda.

The festival’s flagship artistic event was the She Matters Concert. “First conceptualized by Globe-athon, a movement dedicated to building connections with leaders on every continent to help women talk about below the belt cancers, the ‘She matters’ concert was held at Camp Kigali and hosted by the University of Global Health Equity (UGHE). The Rwandan singer, actress, and supporter of domestic violence victims, Nirere Shanel, performed ahead of the evening’s headliner; Grammy award-winning Malian singer, Oumou Sangare, a legendary artist using her platform to advocate for women’s rights. The first edition of Hamwe Festival was attended by the Minister of Health, Dr. Diane Gashumba, Peter H. Vrooman, US envoy to Rwanda, Princess Dina Mired of Jordan, and the Vice Chancellor of UGHE, Agnes Binagwaho.”

In addition to celebrating the role that arts have historically played in the health of people, the Hamwe Festival hosted a Masterclass on Arts and Global Health. The objective was to give participants an opportunity to learn from people working within this nexus about how they use their preferred medium of artistic expression to improve the health of people all over the world whether it be film for advocacy or theater for healing trauma. I opened the masterclass with an introductory lecture on the principles of global health equity. Some topics that were covered during the two-day master class included what it takes to design and evaluate arts in health programs, fund mobilization, and what it means to use arts as therapeutic tools. We hope that this cohort and the future cohorts will keep growing the network of artists and health workers committed to working together to improve health and access to health care for all across the world.
Read more about the Hamwe Festival here: https://ughe.org/hamwe-festival/
Women Leaders in Global Health Conference 2019
November 9-10, 2019

It was an honor for UGHE to host the Women Leaders In Global Health conference for 2019 in Kigali. WLGH 2019 brought together more than 1000 participants from the global health community, with the majority coming from the developing world. All continents were represented and contributed to conversations about changing the face of global health leadership and creating enabling environments for women to thrive in health work. Some themes that were brought up included leveraging innovation to accelerate gender equity in health, the role of men in the fight for gender equity, and the need for continued meaningful collaboration and disruption of the status quo. I was honored to deliver a message of a bright future as I introduced the brand-new Center for Gender Equity at UGHE. The goal of this new center will be to identify and address gender-based barriers to reaching the health goals through community centered research and engagement. We have high hopes that this center will contribute to achieving and advocating for the objectives of the conference and help all of us to keep the momentum.
Watch the highlights video here: https://www.youtube.com/watch?v=TXXEbhLcvbM&feature=emb_title
Read the conference report here: https://ughe.org/women-leaders-in-global-health-conference-2019/wlgh19-proceeding-report/
During the conference, the participants came together to provide insights on how to improve the position of women in global health and conceived a call to action that is inclusive, and concerns all the sectors of global health.
Read the full WLGH 2019 Call To Action here: https://ughe.org/a-call-for-action-from-wlgh19/
UGHE Emerging Leaders Academy
November 8, 2019


Along the sidelines of WLGH 2019, in collaboration with Dr. Modupe Akinola, Associate Professor of Management, Columbia Business School; Dr. Katherine Klein, Edward H. Bowman Professor of Management and Vice-Dean, Wharton Social Impact Initiative; Peter Drobac, Director of the Skoll Centre for Social Entrepreneurship; UGHE brought together an impressive group of 92 young leaders of the health sector, aged less than 35 years old, for a day of initiation to leadership and learning from leaders in global health and entrepreneurship. The goal of this gathering was to facilitate discussions around how to learn to be an effective leader, and equally important, how to be an effective team member. The participants committed to undertake a full online leadership course and upon completion will benefit from a two year mentorship, where they will be paired up with a strong mentor. We hope that gatherings like these will pave the way for more young women and men from the global south to take up space on the leadership tables. The future of global health leadership is truly promising.
Grand Challenges Annual Meeting
October 28-30, 2019

The Grand Challenges Annual Meeting is a convening of over 1000 key leaders from across the global community to share best practices, encourage collaboration, and seek solutions for common challenges. The annual meeting aims to build momentum for global health and development innovation and foster scientific collaboration among international groups and researchers. At this year’s conference in Addis Ababa, along with my Research Associate Mimi Frisch, we presented a poster entitled: UGHE: innovation in medical education. It was a pleasure to share the dream we have for UGHE with others in the field of global health and medical education. During the meeting, the African Academy of Science and the WHO signed a memorandum of understanding to seal a partnership whose goal is leverage innovations and sustainably scale them up to guarantee a healthier and more productive future for Africa. It was a very moving moment that promises to further develop research in Africa.
More about the AAS and WHO partnership here: https://grandchallenges.org/videos
MANOVA Summit on the Future of Global Health
October 16, 2019

The Manova Summit is an annual conference that brings together global health stakeholders from the private, public, academic, and policy sectors to learn from each other how to create the health systems that the future needs. I spoke to them about the importance of looking at innovations as more than just new and shiny technology and products. Innovation is a mindset and can be created through good governance, collaboration, and having a shared common vision. Using examples from the Rwandan health system such as the Zipline drone program, the HPV Vaccine rollout, and the University of Global Health Equity, I emphasized the need to create health systems that foster innovation especially for countries with few resources. Innovations allow us to fly but we also need innovative advocacy in order to be able to bring others on board whether it be our leaders when mobilizing resources, peers when we need partners in implementation, or the communities that we serve because if the community is not convinced of the usefulness of a program or innovation, it is as good as having created nothing.
Read more about the Manova Summit on the Future of Global Health here: https://www.manovasummit.com/
Vermont Oxford Network Annual Quality Congress
October 5-6, 2019

The Vermont Oxford Network is a network with the mission to improve the quality, safety, and value of care for newborn infants and their families through a coordinated program of data-driven quality improvement, education, and research. At the annual VON conference of 2019, I was invited to give a plenary presentation entitled: The Future of Global Health: Equity, Collaboration and Education, as well as a keynote presentation entitled Reducing neonatal mortality: an equity agenda. As part of the keynote presentation, I also participated on a panel with neonatologists from Zimbabwe, Norway, and Puerto Rico to discuss and compare the challenges and successes of neonatal care in our countries. We learned a lot from each other.
Read more about the Vermont Oxford Network Annual Quality Congress here: https://public.vtoxford.org/annual-quality-congress/
Chicago Council on Global Affairs
October 3, 2019

I was honored to be invited by the Chicago Council on Global Affairs to participate in a public dialogue with Brian Hanson about the lessons learned from the rebuilding of Rwanda’s health system following the 1994 genocide against the Tutsi. We spoke about the thousands of health workers and civil servants who came together to build a health system out of nothing and who created a system based on equity and service to the most vulnerable. There is still much work to be done but we are proud of how far we have come together. I am always honored share and learn with the world that it is always possible to build health systems that serve all even starting from scratch.
Read more about the Chicago Council on Global Affairs here: https://www.thechicagocouncil.org/?gclid=Cj0KCQjwjOrtBRCcARIsAEq4rW7N-ZI5IIs9NmG5iUfUbV6U3YYCXQ4lD4DQtQuiSZYzahzeg94kVxsaAnJoEALw_wcB
University of Chicago
October 3, 2019
At the University of Chicago , I was invited by the Center for Global Health to give a presentation on the HPV vaccination launch and rollout in Rwanda, describing the key factors that led to the success of the program. I spoke about the need for innovative advocacy to ensure that the needs of the most vulnerable are met and the importance of community engagement during every step of the development and implementation of public programs. Partnerships between good leadership, scientific advocates, community, and religious leaders were what made this program a success and they are the key to the success of any health program. This talk catalyzed the partnership between UGHE and the University of Chicago and I look forward to what we can accomplish together.
Read more about the University of Chicago Center for Global Health here: https://cgh.uchicago.edu/
Access Challenges Panel on Responsive & Resilient Communities & Health Systems
September 23, 2019

While in New York for the UNGA, I was invited by the Access Challenges (explain) serving as a panelist on the Responsive & Resilient Communities & Health Systems panel. This was an interesting conversation discussing the diverse ways that communities and health systems can be strengthened. I spoke about the importance of global health systems and workforce training through equitable education. Others spoke about health data access, community and reproductive health, health systems level responses to disease, and empowering communities by improving infrastructure. This was a timely conversation to happen while the UN community was committing to working towards Universal Health Coverage. The conference was also attended by WHO leadership and H.E. Amira El Fadil the Commissioner for social affairs for the African Union.
Read more about the Access Challenges conference here: https://www.onecbyone2030.org/
Commonwealth Road Safety Conference
September 3, 2019

I was honored to be invited to speak at the International Road Safety Conference organized by the Towards Zero Foundation and the UK Department of Transportation to make formal commitments towards halving road deaths and serious injuries by 2030. Road related incidents are currently the leading cause of deaths of young people between the ages of 5-29 years. I spoke about why this is a pertinent issue for countries like Rwanda where the majority of the population falls in this age range. This conference brought together some of the leading minds in road safety from all over the world to share best practices and ideas on how to make sure road safety is treated as a priority on a global scale and created a call to action for the global community.
Read more about the International Road Safety Conference here: https://citainsp.org/2019/09/03/international-road-safety-conference-2019/
Masters of Science in Global Health Delivery Graduation – Class of 2019
August 11, 2019



It was truly an honor to give the welcoming address at the 2019 MGHD commencement ceremony. The graduating class of 2019, cohorts 3 and 4, is made up of 46 students from 11 countries – a global class in every sense of the word. Joined by Her Excellency the First Lady of the Republic of Rwanda, Mrs Jeanette Kagame; the Minister of Health, Hon. Diane Gashumba, who was representing His Excellency the President of the Republic, Chancellor of UGHE, Paul Farmer, and Jim Yong Kim, our key note speaker for the day; we congratulated the students for their great achievements and implored them to keep building strong partnerships of good will to make the world better.
The class pledged to lead with intentionality, integrity, and dignity and to maintain the utmost respect for human life and rights as they go out into the world. We are very proud of our newly graduated lions and look forward to all the great things they will accomplish wherever they go.
View more images from the 2019 MGHD graduation here: https://www.flickr.com/photos/183521406@N07/albums/72157710418350046
MGHD Masterclass 2019
August 10, 2019

It was one of my proudest moments to moderate a discussion between the students from our two graduating cohorts and my dear friend and brother Paul Farmer. During this two hour conversation, the MGHD students engaged in discussions on philosophical ideas such as neocolonialism and restorative justice as well as more practical issues like resource mobilisation for better health systems. We also spoke extensively about the role of anger in mobilising the work needed to change the world for the better. The graduating class of 2019 includes doctors, nurses, civil servants, mental health professionals, to name a few, and it gives me great hope to know that they will be leading the charge for better health for all especially the vulnerable.
Read more about the MGHD program here: https://ughe.org/academics/mghd/
ALforHealth Conference
July 19, 2019

I was pleased to be a part of African Leadership Academy’s inaugural healthcare conference, ALforHealth, which was held in Kigali, Rwanda with the aim to build and sustain a network of changemakers who will work hard to change the world with big ideas. I spoke to small groups of young, ambitious African women and men about the work we all for the recovering of the Rwandan health system from the complete destruction of the Genocide against the Tutsi of 1994. Central to this conversation was the role that innovation and research have played in both my own career and the development of my country’s health system.
This conference was in partnership with our university. Later that afternoon, we had the pleasure of hosting a breakout session at the UGHE Kigali Campus to introduce the group to the vision and mission of our organization and discuss what universal health coverage means and how we will achieve it.
Read more about ALforHealth here: http://www.alforhealth.com/
Global Health Corps Training Institute
July 12, 2019

I was thrilled to speak to the new class of Global Health Corps fellows before they went out to start their year of intensive immersion into global health work. I spoke to them about the importance of optimism in the work that we do in global health. Without optimism, we would not have gotten Rwanda from where we were 25 years ago and we will need to stay optimistic for the journey ahead. I was proud to spend the day with the future of global health leadership who set out into the world to do everything with equity in mind. The future is bright!
Read more about Global Health Corps’ work here: https://ghcorps.org/
Health and Humanitarian Logistics Conference
July 10, 2019

The 19th Conference on Health and Humanitarian Logistics, brought together people from various sectors, private and public, to tackle the issue of logistics for health. I joined Dr. Lloyd Matowe, Program Director, Pharmaceutical Systems Africa and Dean of the Faculty of Pharmacy at Lusaka Apex Medical University, Zambia; Ugochi Daniels, United Nations Resident Coordinator- I.R. of Iran, United Nations.Former Head of the Humanitarian Branch, UNFPA HQ; Dr. Henry Kyobe Bosa, Outbreak & Epidemic Senior Public Health Officer, Outbreaks and Epidemics, African Risk Capacity; and Dr. Julie Swann, Department Head & Professor, Department of Industrial and Systems Engineering, NC State University; Co-founder, Center for Health & Humanitarian Systems (CHHS) to discuss different ways to build resilience into our systems through education, early warning systems, and not leaving anyone behind. Applying the principles of implementation sciences with honesty and transparency will support all journeys to success.
Read more about the Health and Humanitarian Logistics conference here: https://chhs.gatech.edu/conference/
The Inauguration of UGHE’s MBBS Program
July 9, 2019

On July 9, 2019, we officially welcomed the inaugural class of medical students to our beautiful UGHE Butaro Campus in Burera, Northern Province, Rwanda. The class is comprised of 30 young and eager minds, of whom 70% are women. All students have made the commitment to work for vulnerable people in need, for at least six years after they finish their training. The education is free. They can work for public sectors, governments, UN, NGOs, etc…and keep all their salary without reimbursing anything as long as their work is in service of the vulnerable in need. The six and a half year bachelor level medical degree, coupled with a masters degree in global health delivery, is heavily grounded. We are very excited to be educating the minds and hearts that will change the way health sciences are taught and health care is delivered around the world, for the better. I gave a lecture introducing them to the history, the mission and vision of UGHE, that they are now a part of and the responsibility they have to upholding the values of equity and community.
Read more about UGHE’s MBBS program here: https://ughe.org/academics/bachelor-medicine-bachelor-surgery/
Kigali Global Dialogue
July 3, 2019

At the inaugural Kigali Global Dialogue, I was pleased to be on a planel of exceptional African health leaders to discuss the intricacies of building strong health systems especially during and post crisis. I was joined by Hon. Dr. Patrick Ndimubanzi, Minister of State, Ministry of Health, Rwanda; Hon. Issa Mardo Djabir, parliamentarian from the Republic of Chad; Rachel Toku-Appiah, Programme Manager, Graça Machel Trust; Freddy Nkosi, Senior Manager, Advocacy & Communications, VillageReach; and Virginia Comolli, Senior Fellow for Conflict, Security and Development, International Institute for Strategic Studies. This Dialogue was a start to what will become an annual convening of minds to tackle contemporary issues surrounding development and growth. We discussed the mutual accountability that concerns government but also NGOs that receive money to care for the vulnerable. They need work with the same efficiency and efficacy during peace and development or during war and unrest. How to do this successfully is part of what we teach at UGHE.
Read more about the Kigali Global Dialogue here: https://www.orfonline.org/orf-kgd/
Taking the Lead on Global Health panel during the Aspen Ideas Health
June 22, 2019

On this panel during Aspen Ideas: Health, I joined Victor Dzau, President of the United States National Academy of Medicine; Robert Newman, Director of Aspen Global Innovators Group; and moderator, Peggy Clark, Executive Director of Aspen Global Innovators Group, to discuss the role of good, effective leadership in the delivery of global health. I spoke about the need for humility, trust, and listening to the people when it comes to delivering health services and leading in general.
Watch the full session here: https://www.aspenideas.org/sessions/taking-the-lead-on-global-health
Reproductive Rights Still a Battleground Panel during the Aspen Ideas Health
June 21, 2019

On this panel during Aspen Ideas: Health, we discussed the way forward for reproductive rights globally. I had the pleasure of joining a remarkable group of women: Leana Wen, MD, President of Planned Parenthood Federation of America, Shadia Elshiwy, MD, Assistant Regional Director for International Planned Parenthood Federation in the Arab World, Aspen Institute Fellow, and moderator, Pat Mitchell – TEDWomen. I spoke about the global nature of the fight for reproductive rights and the power that comes with women being able to have full control over their own healthcare.
Watch the full session here: https://www.aspenideas.org/sessions/reproductive-rights-still-a-battleground
Wellcome Global Monitor Launch
June 19, 2019

At the launch of the world’s largest survey on global attitudes towards science, I had the honor of sitting on a panel with Julie Gerberding, Executive Vice President & Chief Patient Officer, Strategic Communications, Global Public Policy and Population Health, Merck, Mae Jemison, First woman of colour in space and Principal of the 100 Year Starship Initiative, and Imran Khan, Head of Public Engagement, Wellcome. With Jon Clifton, Global Managing Partner, Gallup, moderating we discussed the findings of the survey and their implications on the global community going forward. I spoke about Rwanda’s high levels of trust in vaccines and how we achieved this using a participatory process that involved all stakeholders.
Read more about the Global Monitor Report here: https://wellcome.ac.uk/what-we-do/our-work/wellcome-global-monitor
T20 Summit
May 27, 2019

At the annual Think 20 Summit of 2019, I participated in a panel discussion along Masahiko Kiya (Deputy Assistant Minister, International Cooperation Bureau, Ambassador for TICAD, Ministry of Foreign Affairs of Japan), Sachin Chaturvedi (Director-General, Research and Information System for Developing Countries (RIS)), and moderated by, Gabriel Leung (Dean of Medicine and Helen and Francis Zimmern Professor in Population Health, the University of Hong Kong) discussing recommendations to be made at the G20 Summit regarding achieving Universal Health Coverage globally. The recommendations will be presented at the G20 Summit in Osaka in June. I insisted on the need to create global regulations that protect the developing world against brain drain. The loss of qualified medical professionals to the developed world is a significant obstacle to achieving universal health coverage.
Read more about the T20 Summit here: https://t20japan.org/t20-summit-to-convene-on-26-27-may-in-tokyo/
Exemplars in Under 5 Mortality: Bangladesh workshop
May 2019

In this dissemination meeting, I and my Co-PI Lisa Hirschhorn, along with my team, presented the findings from the Bangladesh Exemplars in Under 5 Mortality case study to the various stakeholders. Together we discussed the validity of the findings and answered questions from the stakeholders who were present at the meeting. We were positively impressed by the responsiveness and the quality of research skills from the ICDDR,B.
SDG3 Workshop: Elevating national research for health priorities to achieve effective scale-up
May 5 – 7, 2019

Co-hosted by UGHE and Wellcome Trust, I was honored to be a part of the team leading this workshop that brought together health research professionals from all over the world to come up with ways we can improve how research is carried out on a global scale. Some of the topics that were covered were: who sets and owns national health sector research agendas, how can we coordinate global health research in a more efficient way, how do we increase the numbers and variety of the people producing quality health research? We agreed that we need to create skills in countries to set their own national health research agendas that respond to their specific needs. Wellcome Trust and WHO will present the report to major global players.
Read more about the Global Action Plan here: https://www.who.int/sdg/global-action-plan/GAP_summary.pdf
Women’s Leadership Summit
April 23, 2019

I was honored to join an incredible group of women at The Rockefeller Foundation Bellagio Center for a few days of reflection, learning from one another, and committing to engaging in regular connected and facilitative leadership as we work towards various global goals. I spoke about the importance of improving access to reproductive health and rights if we are to build a more gender equitable world, not only for women but for everyone.
Read more about the Women’s Leadership Summit here: https://www.patmitchellmedia.com/journal/2019/4/8/connecting-women-leaders-to-accelerate-positive-change
Exemplars in Under 5 Mortality – Senegal workshop
April 14 – 19, 2019
In this dissemination meeting, I and my Co-PI Lisa Hirschhorn, along with my team, presented the findings from the Bangladesh Exemplars in Under 5 Mortality case study to the various stakeholders. Together we discussed the validity of the findings and answered questions from the stakeholders who were present at the meeting. We congratulate the team in Senegal, who stayed until 7pm to finish, for their show of commitment.
Unite for Sight Global Health & Innovation Conference
April 13, 2019

At the Unite for Sight GHIC on April 13th 2019, I gave a keynote address emphasizing the moral imperative for us all to be optimistic on this road to achieve the SDGs. I elaborated on the ways in which optimism has been a large driving force behind the development of my country’s health sector and Rwanda’s progress as a whole. I was also a part of a panel seeking to highlight the importance of responsible engagement and integrity in global health along Jordan Levy, Chief External Relations Officer of Ubuntu Pathways, and Joia Mukherjee, Chief Medical Officer of Partners In Health and Associate Professor in the Department of Global Health and Social Medicine at Harvard Medical School.
Read more about the Unite for Sight Global Health and Innovation conference here: https://www.uniteforsight.org/conference/
Vassar College Visit
April 12, 2019

On April 14th, 2019, I visited the Vassar College campus in Poughkeepsie, New York to meet with President Elizabeth Bradley and some of the diverse student body. It was a pleasure to exchange with the Vassar community on the need for the equity agenda in the development of a health system. The mission of the trip was to cement the partnership between UGHE and Vassar College in educating the future of global health in Rwanda. Vassar will be contributing to the liberal arts part of our curriculum and in turn assuring our students graduate with a better understanding of the world and the societies in which they will work. I also attended a great lecture by Jamaica Kinkaid… I felt the solidarity from the Vassar community when they assisted remotely with me to the commemoration of the genocide against the Tutsi event at UGHE.
Watch the video on the Vassar – UGHE partnership here: https://vimeo.com/330082881
SGO 50th Annual Meeting on Women’s Cancer
March 16, 2019

Image credit: Paula Anastasia
I was invited to be the presidential speaker at the At the 50th Annual Meeting for the Society of Gynecologic Oncology on Women’s Cancers (March 16-19) in Honolulu, HI. In attendance were many professionals from every stage of the gynecologic cancer care spectrum. I spoke about Rwanda’s success with rolling out the HPV vaccine, as well as the need for data driven social and political activism for change. We discussed how lack of trust can lead to missed opportunities such as the underutilization of the minority cancer program in the United States.
Read more about the Society of Gynecologic Oncology here: https://www.sgo50.org/
SDG3 Global Action Plan research accelerator workshop – optimising the global research system
February 22, 2019

Image credit: Rachael Crockett
At this workshop hosted by the Wellcome Trust in London, we discussed strategies that can be employed to produce and use research more efficiently on the road to achieving SDG3. In line with the Global Action Plan: Accelerator 5, ways to increase international collaboration, research agenda streamlining, and recommendations for the future of health research and development were some of the topics of discussion. During this meeting, we made the decision that the next one would take place in Kigali.
Read more about the Global Action Plan here: https://www.who.int/sdg/global-action-plan/GAP_summary.pdf
Fixing the Fundamentals: Lessons from Rwanda’s Healthcare Sector
Published by the Africa Business Conference at Harvard Business School
March 10, 2019

“A good entrepreneur is a good advocate”
In this keynote address to the Africa Business Conference at Harvard Business School on February 16, 2019, I described the successful strategies taken in the Rwandan health sector to rebuild and work for equity in the time since the genocide in 1994. I elaborate on ways in which a government can make great progress by planning and acting as a business, and I describe how the private sector has an essential role to play in human development and health for all.
Watch the full keynote address
Leadership and Management: Critical Barriers to Improving Health Outcomes

“Former CDC Director William Foege stated, ‘the lack of management skills appears to be the single most important barrier to improving health throughout the world.’ Strong leadership and management capacity are essential ‘force multipliers’ within health systems that increase the prospect of better health outcomes. However, without consensus on definitions and investment in robust evaluations to measure impact, evidence isn’t available to inform decisions regarding prioritization, adaptation, or scale-up. Panelists will describe efforts to build leadership and management and discuss the pressing need to create a shared agenda for professionalization of leadership and management education in the global health context.”
It was a privilege to start International Women’s Day with a panel composed of such knowledgeable women, Amy Lockwood, Strategic Advisor to AIDS Research Institute & Center for Global Health Delivery and Diplomacy at UCSF’s Institute for Global Health, Heather Anderson, Senior Vice President of Programs at Global Health Corps, Erika Linnander, Lecturer in Public Health (Health Policy) and Director of the Global Health Leadership Initiative at Yale University, and Erika Willacy, Program Lead for the Improving Public Management for Action (IMPACT) Training Program at CDC.
Read more about CUGH 2019 here: https://www.cugh2019.org/
Planning and Action for Cervical Cancer Elimination in Rwanda: Lessons Learned from Sustaining Success and the Way Forward
Panelist on “Eradicating Deaths from Cervical Cancer” at the 7th Annual Symposium on Global Cancer Research
March 7, 2019

In this panel presentation, I delivered a keynote address describing the planning and implementation of HPV vaccine in Rwanda and efforts for cervical cancer elimination. I shared lessons learned and next steps for other countries and for international actors regarding cervical cancer elimination and delivering quality cancer care in developing countries and around the world.
Read more about this symposium here: https://www.cugh2019.org/cancer
Global Public Health Today and Tomorrow Panelist at Festival of the Arts Boca
March 4, 2019

“Two esteemed experts on global health issues – one American, one Rwandan – offer a panel discussion on the state of world health.
Dr. Agnes Binagwaho, Vice Chancellor of the University of Global Health Equity, an initiative of Partners in Health, brings her perspective as a practicing physician, scholar, and government health official, including having served as Rwandan Minister of Health. She is active in advocacy and political mobilization on behalf of women and children, in Rwanda and worldwide. Partners In Health is focused on changing the way health care is delivered around the world.
Thomas Bollyky offers the insights of a scholar and author, having directed the first Council on Foreign Relations-sponsored Independent Task Force devoted to global health, and he also is the author of Plagues and the Paradox of Progress: Why the World is Getting Healthier in Worrisome Ways.
The panel will be moderated by Dr. Felicia Knaul, Director, Institute for Advanced Study of the Americas and Professor, Miller School of Medicine, and it will be introduced by Boca Raton Regional Hospital President and CEO Jerry Fedele.“
Read more about the Festival of the Arts Boca here: https://festivalboca.org/
Global Health Equity and the Research University: An Update from Rwanda Panel discussion with Dr. Paul Farmer and moderated by Dr. Salmaan Keshavjee
February 14, 2019 at Harvard Medical School

In this panel discussion, Paul Farmer and I share our experiences and secrets for success in global health delivery. The central motivation is focusing on those who have been excluded, and, in doing so, you will reach every person. Dr. Farmer and I also discussed how the University of Global Health Equity will solve a leadership, research, and implementation science gap in global health delivery by educating our students in the principles of equity, One Health, and evidence-based decision making.
Interview and Discussion at Harvard School of Public Health
February 14, 2019

On February 14th, 2019, I was interviewed by Dr. Joseph Rhatigan, Associate Professor in the Department of Global Health and Population, at the Harvard School of Public Health regarding my experience working for health and development with an equity agenda. I engaged with Dr. Rhatigan and his students in a discussion of the nuances of implementing this equity agenda and shared my experiences as a global health fighter, public servant, and now Vice Chancellor.
Read more about the Harvard School of Public Health’s academic offerings
Screening of Bending the Arc and Moderated Discussion at The Conduit in London
Screening and discussion on February 11, 2019
On February 11, 2019, I participated in a screening of Bending the Arc and a post-screening panel discussion with Dr. Peter Drobac, Director of the Skoll Centre for Social Entrepreneurship at the Said Business School. Our discussion centered around the lessons from the film and the lessons we can draw from the activism and advocacy of Partners In Health that resulted in systemic change in many countries.
Optimizing leadership and organization in healthcare: Restructuring health systems to ensure universal coverage
Speaker at the Rhodes Healthcare Forum at Oxford on February 9, 2019

“In 2019, our theme is ‘From Surviving to Thriving’. We rightly celebrate our remarkable progress to reduce death and disease worldwide. Our focus must now shift to goals beyond just reducing mortality, to create a future where everyone can enjoy thriving health. We must pursue wellbeing, prevent disease, reduce inequality and seek justice for all. We will discuss opportunities and approaches in technology, epidemiology, public health, drug discovery, biomedicine and policy to promote global thriving
health.
We have invited experts and innovators in to bring depth to these discussions. Scholars will be encouraged to apply the ideas generated over the weekend in initiatives spanning their time at Oxford and beyond.”
In this talk I outlined successful strategies for optimizing health systems for the benefit of all citizens, with the goal of universal health coverage, using Rwanda as an example.
Opening Address at AMP Health’s Leadership Lab Welcome Reception
January 27, 2019

I spoke to the participants in the Aspen Management Partners for Health Leadership Lab at the kickoff of their intensive training in Rwanda about the importance of leadership and management in Rwanda’s journey to health excellence and in achieving the goals for Primary Health Care across Africa. UGHE and AMP Health are seeking to build strong health systems of the future and are forging the potential for even stronger collaboration. AMP Health works in partnership with Ministries of Health across Africa by strengthening leadership and management capabilities to accelerate achievement of the shared goals of the Primary Health Care (including Community Health), Universal Health Coverage, and the health-related Sustainable Development Goals.
Welcome Address at UGHE’s Butaro Campus Ribbon Cutting Ceremony Address
January 25, 2019

On the event of UGHE’s official Butaro campus launch on January 25th, 2019, I spoke to our esteemed guests and colleagues to share our collective story of Rwanda and PIH’s journey in health equity, our thanks to the community and local and national government for their support, and our vision for this university and the field of global health delivery.
Promoting research and Education towards Hepatitis Elimination in Sub Saharan AfricaCo-moderator of session with Professor Phil Cotton
December 12, 2018

Professor Phil Cotton, Vice Chancellor of the University of Rwanda, and I led a lively discussion about the promotion of research and education for Hepatitis C virus elimination in Rwanda and the world. This event was convened to mark the launch of Rwanda’s Hepatitis C virus elimination plan.
Leadership Master Class at the Gavi EPI LAMP Closing
Interviewed by Erika Linnander of Yale University’s Global Health Leadership Initiative

I spoke with the participants in the Gavi EPI Leadership and Management Program on the occasion of their graduation from the program to deliver a call to action for the health sector leaders to continue to develop their leadership and management skills and implement innovative projects in immunization.
Observations and Expectations for G20 Universal Health Coverage: An African Perspective Presented at T20 Inception Conference
December 5, 2018 in Tokyo, Japan

I was invited by the T20 Japan Secretariat, in preparation for the G20 meetings in Japan in 2019, to discuss global cross-cutting issues and advise on roadmaps for policy recommendations to the G20. At this conference, I shared my views on universal access to care for the developing world and emphasized the importance of not doing “one package” for the world but instead to move forward based on capacity of countries, keeping with high expectations for global progress.
Safe surgery: collaborating to increase access and improve outcomes
Panelist at UBS Global Philanthropy Forum
November 30, 2018 in St. Moritz, Switzerland

On this panel I encouraged all actors to align with the Lancet Commission on Global Surgery recommendations and met with philanthropists who are eager to help countries around the world to help in this effort. I offered advice on how to do this in an integrated systemic manner. I also spoke about my experiences in building a health sector and working within a leadership culture that has an equity mindset.
Speaker/panelist at World Innovation Summit for Health
November 13, 2018 in Doha, Qatar

On this panel, we engaged in a lively discussion about the need for distinctions and cooperation between measures of social capital and human capital. I argued that social cohesion is a more important factor for mental health than economic potential and that this is key to understanding and addressing mental health challenges for children and adolescents.
Equity in Academic Global Health Partnerships Panelist at Women Leaders in Global Health Conference
At the London School of Hygiene and Tropical Medicine
November 9, 2018

On this panel, we discussed inequity in academic partnerships as a serious problem that needs to be addressed. We came together to talk about the barriers and opportunities for more equitable partnerships in the interest of advancing science and health for all. I spoke about the need to raise awareness and build partnerships and relationships with other institutions in the developed and developing world in order to combat structural violence and “-isms” that prevent true gender equity and fair partnerships in academia around the world.
Read more about this conference
Taking global health work from silos to systems: How might we align incentives across sectors?
Panelist at Prescription for Progress: The essential role of partnerships in strengthening health systems
October 30, 2018 at Devex in San Francisco, California

In this panel, I argue for stronger partnerships between the public and private sectors and communities and push all stakeholders to take risks on innovation. To move forward for equitable healthcare access for all and effective health systems, we need to gather everyone involved around one table and one vision for health and development, and stop treating governments like children who are out of touch with the needs of their people. This requires greater accountability from all parties.
Watch the full panel (43:37 – 1:16:48)
Reimagining health education for quality service for all is a good business
Presenter in Med 285 course at Stanford University
October 24, 2018

I gave a lecture to the Stanford Distinguished Careers Institute Fellows about why quality health education is a smart business strategy – because less money is spent on economic development when funds are spent disproportionately on disease. When populations are healthier, more economically productive people are able to work and build their local economies, leading to overall economic development. This was a vibrant, multigenerational group with a wide range of expertise from around the world.
Read more about this institute and fellowship
Quest for an effective health system: 20 years of Rwandan experience Grand rounds presentation at El Camino Hospital
October 23, 2018 in San Francisco, California
This presentation focused on accelerating access to health by embedding trust between clients and service providers, and the need to cultivate that trust among community members. I described the experience of Rwanda in rebuilding our health sector through individual and community trust in the leadership as a key tool for implementing needed health reforms.
Address to Students of the Castilleja School
October 22, 2018 in Palo Alto, California

I was delighted to speak with this young group of women about my career in global health. These children were truly thinking strategically about how to find solutions for being productive in the communities in wish they will work in the future when they are young professionals. It showed me again how important it is to receive quality education that encourages this type of strategic thinking and a sense of social justice in students.
Read more about the Castilleja School
Rwanda’s Health Care Transformation: A Model for Success
Featured speaker
October 18, 2018 at the World Affairs Council of San Francisco

In this “salon talk-style” conversation with Krista Donaldson, CEO of D-Rev, I discussed what it takes to build an equitable health system and how human development is needed to sustain economic development. I shared stories of using technology (like Twitter) to communicate with beneficiaries and call out big health multilateral organizations to reconsider their inaccurate Rwanda data and how to use “reverse innovations” and innovative partnerships for better health outcomes for all.
The Role of Educational Institutions in Creating Social Change
Fireside chat
October 16, 2018 at the Harvard Club of San Francisco
In this presentation, I described why we need to revisit educational systems in order to create social change for better service delivery. I examined if the training provided today appropriate to reach the SDGs, why we need to take a global health approach, how Rwanda’s brought about progress using knowledge-based development strategies (and the consequences of not doing so), and how we can change access to education to foster positive social change.
Rwanda’s Journey to Reducing Under-5 Mortality: Embedding equity in child health
Keynote address at the 2018 Summit for Pediatric Global Health, Mass General Hospital for Children
October 15, 2018 in Boston, Massachusetts

In this address, I shared Rwanda’s journey for under-5 mortality reduction – a journey of collaboration and visionary leadership to ensure healthy lives for kids and for all. We did this through an equity agenda and evidence-based decision making – as we did with everything in the health sector – as a key strategy for saving lives and reducing morbidity.
Screening of Bending the Arc and Post-screening Discussion
October 12, 2018 at the Dickey Center at Dartmouth College

After the screening of Bending the Arc, students, faculty, and staff engaged with me in a discussion about bringing stakeholders around a singular vision for better health outcomes for all.
Meeting of the Friends of Vision group at the United Nations
Speaker on October 11, 2018 at the United Nations Headquarters in New York

At this meeting, to mark World Sight Day, I spoke at the founding meeting of the Friends of Vision group at the United Nations, which includes Clearly, Ambassador Webson, UN Permanent Representative of Antigua & Barbuda, and the International Agency for the Prevention of Blindness. I shared lessons learned in Rwanda from working with Vision for a Nation to fight for universal access to eye care.
Invest, Innovate, Empower: Marshalling Collective Action to Drive the Women’s Health Research Agenda Forward
Panelist at the Magee-Womens Research Summit
October 9 2018 in Pittsburgh, Pennsylvania

On this panel, we discussed the persistent gender inequity that leads to both a lack of women in research and a lack of research about women’s specific health needs. We need to increase women in STEM fields – in representation as researchers, which will hopefully also increase representation in research. Building a sustainable health system requires the competency to design and implement policies and legal frameworks that are evidenced-based and utilize available data but if your data misses half of your population’s needs, then your decisions will not be truly evidence-based. I argued for shifting the health research agenda towards gender equity, elaborating on lessons learned from HIV/AIDS research advocacy and proposed the way forward to increase resources for women’s representation in health research.
Reducing the Rate of Maternal and Infant Mortality: Trends, Challenges and Opportunities Panelist at the Magee-Womens Research Summit
October 9 2018 in Pittsburgh, Pennsylvania

Each country faces different social determinants of health that must be addressed to solve clinical issues. Not doing that will make you fail to create the health system based on inclusion, equity, and quality for all, responding to the needs of the people in their community. In this panel, I discussed how to realistically address maternal and infant mortality – which in US means you must have honest discussions about institutional racism, and in other contexts means facing your unique challenges and threats to women’s health head-on.
Forum on Neglected Tropical Diseases Panelist at the Access Challenge’s Universal Health Coverage Conference 2018
September 24, 2018 in New York

I joined other global health leaders on this panel to discuss NTDs, which affect 1.5 billion people globally, and why we need to sustain ambition toward Universal Health Coverage to beat these diseases. I spoke the importance of integrating NTD care more strongly into primary health care structures, building country capacity, encouraging leadership to tackle these illnesses, and using data to measure successes to incentivize action towards eliminating NTDs.
Read more about the Access Challenge
The Humanitarian Use of Drone Technology: Innovations for Health in Rwanda
Presenter at Hong Kong University of Science and Technology
September 20, 2018

In this presentation, I described Rwanda’s successful implementation of drone technology for delivery of needed health supplies to remote locations, greatly reducing delivery delays and, ultimately, saving lives in difficult-to-reach areas. I illustrated how the use of drones can be a great innovation for health service delivery. It is a lesson about how Africa can leap into the future and solve problems using science the most advanced technology to solve persistent health issues.
Read more about Rwanda’s drone delivery program
Nationwide Rollout of the HPV Vaccine in Rwanda: Embedding equity in cancer control planning Presidential plenary speaker at the International Gynecological Cancer Society Meeting
September 15, 2018 in Kyoto, Japan
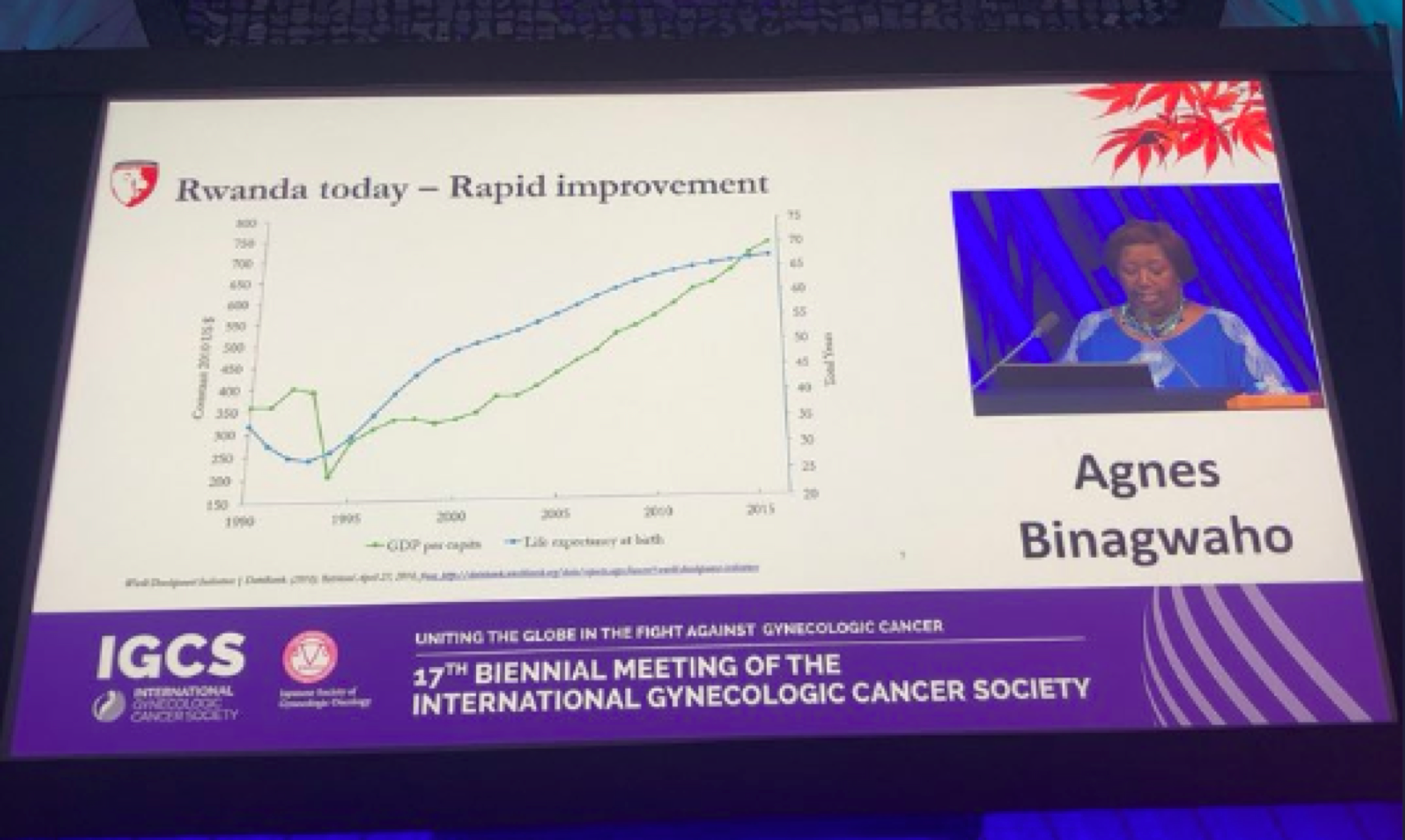
I was invited to deliver the Presidential plenary address at the IGCS 2018 meeting about Rwanda’s national HPV vaccination program: the need, advocacy efforts, rollout, controversies, and the larger context of cancer treatment in our setting. I also shared lessons learned and next steps. This example is a perfect case study of Rwanda’s practice of early adoption, of innovating for health, and of putting the most vulnerable citizens at the forefront of our minds when implementing health interventions.
Exemplars in under-five mortality reduction: A case study of implementations strategies and contextual factors in Rwanda
Research presentation at Rwanda Ministry of Health 2018 Health Research and Policy Day
August 24, 2018 in Kigali, Rwanda

At this Health Research and Policy Day, I presented the preliminary results of a novel research project that involves using implementation science methods to seek out transferrable knowledge for reducing under-5 mortality from countries that have exceeded expectations in this key health indicator. Rwanda was the first of many countries where this research was conducted, and we plan to use this methodology to develop a toolkit for countries who wish to successfully reduce child mortality.
Promotion of multisectoral partnerships for the prevention and control of non-communicable diseases
Presenter/panelist at the Interactive Hearing as part of the preparatory process toward the Third High-Level Meeting of the General Assembly on NCDs
July 5, 2018 at the United Nations Headquarters, New York.

In this interactive discussion, we discussed the opportunities and challenges of engagement with the private sector, academia, civil society, and communities for the prevention and control of non-communicable diseases. I argued that private, public and community partnerships are key to reducing the burden of NCDs and efforts to do so in Rwanda have been possible for us because of the government’s support of community health centers, new health interventions, and other private and public health organizations within the country. We know that civil society has an essential role to play, alongside government and business, in tackling NCDs in Rwanda, and around the world. I also argued that the private sector has shirked their responsibility for the current state of NCDs and their role in creating obesity- and smoking-related illnesses. To move into an era of real partnerships, the private sector must employ real accountability, transparency, and truth-telling.
Health Systems Strengthening: The Experience of Rwanda
Presenter/panelist at Global Health Corps Training Institute
Yale University on July 2, 2018

At this GHC Training Institute, I spoke to the new GHC Fellows about health systems strengthening and the building blocks of health systems needed to foster human development and break the cycle of poverty and disease. I shared my experience in the Rwandan health sector and the revolutionary solutions we employed in leadership, data collection and use, community engagement, and equitable health delivery in order to achieve more for the health of our people. After my presentation, I engaged in a panel discussion with Dr. Prabhjot Singh about how these young professionals could work in their fellowships to reduce health inequities.
Read more about the GHC Training Institute
The U.S Vs The World: Who Has The Best Healthcare System?
Published by Aspen Ideas on June 22, 2018

VIEW PHOTOS FROM THE EVENT HERE:HTTPS://WWW.FLICKR.COM/PHOTOS/60463478@N08/SETS/72157670396805928/WITH/29082213948/
“You’ll go nowhere if you don’t create the system to provide good services.”
According to the commonwealth fund in a recent report, the united states health care system does not perform at the level that should be expected based on how much is spent, particularly when it comes to outcomes, access, and equity. In this panel, I describe the approaches we took in the Rwandan health sector to reduce inequity and increase access to health for all, resting on principles of inclusiveness (“whatever program you do, make sure you leave no one out”), addressing the social determinants of health, and a governance structure that puts human development first. These practices have allowed us to make great strides with little money, which is a stark contrast to the united states health system. I share these lessons learned from Rwanda, and around the world, about equitable health delivery and how we are educating future global health professionals in these lessons at the university of global health equity.
SPEAKERS: AGNES BINAGWAHO, DAVID BLUMENTHAL, TAKAO TODA
WATCH THE FULL EVENT HERE:
HTTPS://WWW.ASPENIDEAS.ORG/SESSION/US-VS-WORLD-WHO-HAS-BEST-HEALTH-CARE-SYSTEM
Fighting Cancer in Africa
Published by Aspen Ideas on June 22, 2018

In this panel, I discuss the misconceptions surrounding cancer care in Africa and the barriers to effective treatment that still exist for African cancer patients. I tie these barriers to lack of political action on the part of local and national governments on the continent; pervasive stereotypes about why Africans do not or cannot seek treatment in time; lack of effective advocacy for non-communicable diseases; and biases among international policymakers, advocates, and researchers regarding what is “appropriate” or possible in cancer research and treatment in Africa. These barriers align with our understanding of the social determinants of health and the continuing structural violence that African cancer patients face when seeking diagnosis or treatment for cancer. To adequately address the rise in cancer incidence in Africa, we will need to embrace task-shifting for cancer care because, as i say during this panel, “cancer is too serious to leave in the hands of doctors only.” This is the lesson we teach at UGHE, that there is a need to be disruptive and to do business as “unusual”, which means being radical in the way we educate health professionals about cancer and not accepting of the status quo.
SPEAKERS: AGNES BINAGWAHO, RICHARD BERKE, GARY REEDY, KWANELE ASANTE
LISTEN TO THE EVENT: HTTPS://WWW.ASPENIDEAS.ORG/SESSION/FIGHTING-CANCER-AFRICA
VIEW PHOTOS FROM THE EVENT HERE:
HTTPS://WWW.FLICKR.COM/PHOTOS/60463478@N08/SETS/72157695109857032
ENOUGH: Making 2018 The Year For Action and Impact on NCDs
Published by the NCD Alliance on May 21, 2018
In this panel, I shared my perspective on how to make the un NCDs high level meeting count, stressing the importance of integrating services into existing systems, utilizing lessons learned from previous large-scale disease responses (HIV/AIDS, for example), and leaving no one out of benefit. Addressing NCDs will require a collaborative, multisectorial response that attacks NCDs from every side – health, education, governance, society, and more.
WATCH THE FULL PANEL EVENT HERE:
HTTPS://WWW.FACEBOOK.COM/NCDALLIANCE/VIDEOS/644567029220363/
READ MORE ABOUT THE 71ST SESSION OF THE WORLD HEALTH ASSEMBLY HERE:
HTTPS://NCDALLIANCE.ORG/NEWS-EVENTS/NEWS/NCDS-ON-THE-AGENDA-AT-THE-71ST-WORLD-HEALTH-ASSEMBLY
The Lazarus Effect, 15 Years Later
Published by The George W. Bush Presidential Center on May 9, 2018
In this panel, (06:00 – 51:45) on the 15 year anniversary of PEPFAR, I discussed the impact of the program in Africa and the role PEPFAR played in turning the tide against HIV/AIDS in Rwanda.
Panelists: former Rwandan minister of health prof. Agnes Binagwaho, key architect of PEPFAR Ambassador Mark Dybul, m.d.
Washington post columnist Michael Gerson watch the entire panel presentation here: https://www.bushcenter.org/exhibits-and-events/events/2018/05/engage-lazarus-effect
African Women’s Leadership Conference at Wellesley College
Published by Wellesley College on April 13, 2018

On march 8th, 2018, I spoke about the challenges faced by African women in the health sector at the African women’s leadership conference organized by Wellesley college. I began my talk by reminding the audience that Africa as a continent has been misrepresented on the map for so many years, where it is made to appear smaller than it is. I went on to talk about how difficult it is for African women to move up the ladder as leaders in healthcare and other sectors such as politics. I mention the false perspective society has of women’s ability to perform due to their biology. My talk ended by highlighting the great achievements that have been accomplished because of women’s leadership and by encouraging African women and women in general to take a stand and show the world that we, women, can be both mothers and leaders in this world.
WATCH THE FULL TALK HERE: HTTPS://WWW.YOUTUBE.COM/WATCH?V=EVUW3KTDZ10&LIST=PLFWQ1G8JNXN9SJ3G4BZK6VK25_X3WKQ8J&INDEX=11&T=0S
FOR MORE INFORMATION ABOUT THE CONFERENCE, PLEASE VISIT: HTTPS://WWW.WELLESLEY.EDU/AWLC#
FOR MORE INFORMATION ABOUT WELLESLEY COLLEGE PLEASE VISIT: HTTP://WWW.WELLESLEY.EDU/
Oxford Union Debate: The Role of Universities in Creating Social Impact
Published by Skoll Centre for Social Entrepreneurship on April 12, 2018

In this debate at the historic oxford union, i argue against the proposition that “universities lack the necessary ‘proximity’ to be effective agents of social innovation in the 21st century.” I make the case that universities are increasingly using pedagogy that encourages students to engage with communities and seek innovative solutions that can be sustainably implemented in poor, rural areas. I also note that universities are and will continue to be convening spaces for the exchange of ideas, which is only made ever easier by technological advancements and communications connectivity. These are the tools and values of the university of global health equity, where I serve as vice chancellor, which is truly “walking the walk” when it comes to proximity to those we have committed to serve.
WATCH THE FULL DEBATE HERE (I SPEAK FROM ~34:00 – 43:30): HTTPS://WWW.FACEBOOK.COM/SKOLLCENTRE/VIDEOS/2262091323817330/
TEDMED Talk: DR. Agnes Binagwaho
Published on the TedMed Youtube Channel on April 5, 2018

In this TEDMED talk, I shared my personal journey as a passionate healthcare provider. I shared about my love of medicine, my family’s move from Rwanda to Belgium in the years before the genocide and my later return to my homeland after the devastating 1994 genocide against the Tutsi. I shared about the hardships I faced after making such decision and the rewarding fruits of my hard labor. I went from being a regular clinician in Rwanda, to running the national aids control commission, to being appointed as permanent secretary to the minister of health and to later becoming the minister of health. Through my journey, I played a major role in the transformation of Rwanda’s healthcare sector, a work that now serves as a model to both developed and developing nations. My journey has led me to my current position as the vice chancellor of the university of global health equity (UGHE).
WATCH MY 2017 TEDMED TALK:
HTTPS://WWW.YOUTUBE.COM/WATCH?V=3GV_UZIFMI8
FOR A Q&A BLOG PUBLISHED FOLLOWING MY TALK PLEASE VISIT:HTTPS://BLOG.TEDMED.COM/QA-AGNES-BINAGWAHO-RWANDAS-FORMER-MINISTER-HEALTH/
CIFAR Women in Leadership Workshop 2018
On March 22, 2018 at Hotel de Mille Collines in Kigali, Rwanda

On march 22, 2018, during the CIFAR’s women in leadership workshop that took place at hotel de Mille Collines, I presented as a keynote speaker about “women’s leadership in science: global challenges and the way forward.” In this presentation, I touched on the importance of fighting against brain drain, to prevent current and future African scientist from leaving the continent in search of better paying jobs from the western world or elsewhere. I also explained how gender inequity is a global issue and how there is so much that can be done to prevent it such as investing in girls education or establishing institutions like the university of global health equity (UGHE) in places where education is most needed. I ended my talk by highlighting UGHE and its mission to create the next generation of global health professionals who are being instilled with a passion to serve and advocate for the most vulnerable. Following my talk, I joined a panel of five other women to discuss more deeply about the challenges that are inhibiting women leaders in science from making progress and how those challenges can be prevented.

FOR MORE INFORMATION ABOUT THE WORKSHOP PLEASE VISIT:
HTTPS://WWW.CIFAR.CA/EVENTS/WOMEN-IN-SCIENCE-LEADERSHIP-WORKSHOP-2018/
FOR MORE INFORMATION ABOUT THE CANADIAN INSTITUTE FOR ADVANCED RESEARCH (CIFAR) PLEASE VISIT: HTTPS://WWW.CIFAR.CA/
Advancing Global Health With Tech
Published by Techonomy on November 14, 2017

In this panel we discuss the development of technology as an absolute and urgent priority to advance global health if we want to reach the sustainable development goals by 2030. I argue that this is true, but we need to accompany technological advancement with the development of social capital and we need to purposely bring technology to the most vulnerable members of the communities in which we work.
WATCH THE FULL VIDEO AT:
HTTPS://TECHONOMY.COM/CONF/TE17/TECH-HEALTH/ADVANCING-GLOBAL-HEALTH-TECH/
Message Foe Members Of The Task Force On Global Advantage
Published by Mount Sinai Health System on September 12, 2017

In this video, I speak about the progress Rwanda has made by highlighting different programs that have contributed greatly to the development of the healthcare within the country in order to support the health of the people. Such programs include community health workers (CHWs) and other policies that were implemented under my leadership.
WATCH THE FULL VIDEO AT: HTTPS://WWW.YOUTUBE.COM/WATCH?V=BMOVUYJHSAI
Healthcare Quality
Published by Harvard X on June 28, 2017

Quality needs to be at all stages of the chain of health service delivery, from patient participation, to infrastructure, to proper use any of the tools necessary for clinical services, to name a few …
WATCH THE VIDEO HERE:
HTTPS://WWW.YOUTUBE.COM/WATCH?V=LS3N6FQ25MW
TO LEARN MORE ABOUT HARVARD X, PLEASE VISIT:
HTTPS://HARVARDX.HARVARD.EDU/WHO-WE-AREAND THE FREE ONLINE COURSE, “IMPROVING GLOBAL HEALTH: FOCUSING ON QUALITY AND SAFETY”: HTTPS://BIT.LY/2NHVMJR
What’s Next in Global Health
Published by the Aspen Institute on June 24, 2020
This year marks the 100th anniversary of the 1918 Spanish influenza pandemic, which killed more people than world war I. In this panel, we discuss how to better use the lessons learned from the past to face “global health threats of today”: the next global pandemic, non-communicable diseases, climate change, the refugee crisis, and many other emerging killers.
SPEAKERS ON THE PANEL: AGNES BINAGWAHO, STEVE DAVIS, MARK SMOLINSKI, AND MICHAEL MYERSMODERATOR: OLGA KHAZANWATCH THE VIDEO HERE:
HTTPS://WWW.YOUTUBE.COM/WATCH?V=GVC6SBIB7WM
TEDxSkoll: Healthcare For All Is The Duty For All
Published by TEDxSkoll on April 19, 2017

In this talk, I explain the importance and power of speaking the truth even when there are numerous forces working against you. I detail the history of my country, Rwanda, as I struggled to make sure that the rest of the world was aware of the true nature of the devastating situation there. Through my experience as a Rwandan who came back to help rebuild her country, I describe why every life is worth fighting for because “being healthy is an economic asset for families, communities and countries.” This is why an institution like the university of global health equity (UGHE) is so vital as it sets out to educate all, starting with those in the most impoverished areas. I explain my belief that by standing in solidarity with the most vulnerable, we will always be able to promote truth.

WATCH THE TALK HERE:HTTPS://WWW.YOUTUBE.COM/WATCH?V=0ONRNMM4V-I
Blessed Unrest: A Theory Of Change
Published by Skoll.org on April 8, 2017

No global health fighter should be satisfied. Dissatisfaction and unrest will animate them and give them the energy needed in their quest for social justice and better access to quality health services for all.
As the Skoll world forum looks to create common ground, in this panel, I explore with independent storytellers and social entrepreneurs how dissatisfaction can fuel positive changes. We discuss the truly global nature of our work and the work that is described in the film bending the arc. I also discuss my experiences of returning to Rwanda after the genocide against the Tutsi and averting the potential spread of Ebola to Rwanda, and the role of anger in being a global health fighter.
WATCH THE FULL PANEL DISCUSSION HERE
(MY PARTICIPATION FROM ~35:00 – 1:15:00):
HTTPS://WWW.YOUTUBE.COM/WATCH?V=9DOLEODDUNU
Universal Health Coverage in Low and Middle Income Countries

In this video, I share my thoughts on the importance of the underlying principles that are key in building and implementing Universal Health Coverage (UHC). UHC is a crucial aim of social justice and the basis for each person to access equitable, quality, sustainable care.
Here is the link to watch the lecture:
http://drive.google.com/file/d/0BwaFF5isjZdBVHZUZ0hLdHZScVE/view
The Quest for Universal Health Coverage in Low and Middle Income Countries
Published by Johns Hopkins University, Maryland, USA (Filmed in Kigali, Rwanda) on April 4, 2016
I gave a guest lecture titled “The Quest for Universal Health Coverage in Low and Middle Income Countries” for Professor Afsan Bhadelia’s Johns Hopkins University undergraduate public health course. This video displays a part of the rich discussion the students and I had during the Q&A following the lecture.

Here is the link to watch the lecture Q&A:
http://drive.google.com/file/d/0BwaFF5isjZdBcW5DVXdGX0hVX0k/view
Building Resilience for NCDs: Integration in Basic Care
Published by Yale University, School of Public Health, Connecticut, USA (Filmed in Kigali, Rwanda) on March 28, 2016
On March 28, 2016, I gave a guest lecture titled “Building Resilience for NCDs: Integration in basic care” followed by a Q&A in Dr. Nicola Hawley’s Yale University School of Public Health course, “Global Non-Communicable Disease.” The Masters-level students were from various departments across Yale University- including public health, epidemiology, infectious diseases, anthropology, and management.

Here is the link to watch the lecture:
http://drive.google.com/file/d/0BwaFF5isjZdBOE0tR3A0Vi14WEE/view
Accepting the 2015 Roux Prize from the Institute of Health Metrics and Evaluation (IHME)
Washington DC, USA on October 21, 2015
On October 21, 2015, I was deeply grateful to represent Rwanda in receiving the Roux Prize from the Institute of Health Metrics and Evaluation (IMHE). We received this esteemed award for our health sector’s use of Global Burden of Disease (GBD) data to make evidence-based decisions around improving neonatal health in Rwanda and, though this, decrease neonatal mortality and reduce suffering among the youngest in our population. Read more about the Roux Prize and theInstitute of Health Metrics and Evaluation (IMHE) here: http://www.healthdata.org/news-release/dr-agnes-binagwaho-minister-health-rwanda-wins-roux-prize-using-data-improve-rwandan
Watch full video here: https://www.youtube.com/watch?time_continue=3&v=fqY9YQ8-M5o&feature=emb_title
Guest on the Big Q (TV Station)
Published in Kigali, Rwanda on October 1, 2015
On October 1, 2015, I was invited to be interviewed on the Big Q, a television show, to discuss health. Watch the recorded videos above.
Speaking About Health and Safety on Work Day in Bralirwa Gisenyi
Gisenyi, Rwanda on May 1, 2015
On May 1, 2015, I spoke to the community of Bralirwa in Gisenyi, Rwanda about health and safety on the annual holiday Umunsi w’umurimo, or “Work Day” in our national language of Kinyarwanda. On this day, we take time as a community to discuss employment, workplace safety, and new innovative ideas.
Inauguration of Children’s Week
Stockholm, Sweden on April 19, 2015
On April 19, 2015, I was honored to speak about the principals of building a system to promote child health in Rwanda, discussing how the future is in our hands.
Featured on #1o1RW with Eugene Anangwe
Kigali, Rwanda on August 25, 2014
On August 25, 2014, I was invited to be a guest on “One on One” with Eugene Anangwe on 89.7 Contact FM here in Kigali to discuss Rwanda’s position on Ebola related issues and other issues in the health sector. It was a fun experience and I hope many were able to listen in for the great conversation!
Dartmouth Lecture: “Building a Health Sector Alongside a Nation”
Dartmouth College, New Hampshire, USA, on July 23, 2014
On July 23, 2014, I was invited to speak at Dartmouth College to give a presentation on how my Rwandan colleagues and I have built the health sector alongside the development of our nation, led by His Excellency President Paul Kagame of the Republic of Rwanda. As I share in my lecture, a health sector must be integrated into the broader development of a country. Here in Rwanda, we are guided by our national development plan, Vision 2020, and our Economic Development and Poverty Reduction Strategy. Each of the strategic plans of the sectors within the government, including the health sector, are aligned with these overall, comprehensive national plans in order to ensure that we are all moving forward together in harmonized, complimentary efforts.
Giving the Inaugural Address at the 3rd National Food and Nutritional Summit
Kigali, Rwanda on February, 2014
On February 18, 2014, I was honored to give the inaugural address at the 3rd National Food and Nutritional Summit here in Kigali. Learn more about the Summit and the conversations we had here: http://www.moh.gov.rw/fileadmin/templates/Summit3/48_Cosensus_Statement.pdf
Voice of Africa Interview: Perspective On U.S. AIDS New Initiative To Increase Research For a Cure For HIV
Published by Voice of Africa on December 3, 2013
Here, on December 3, 2013, I was invited to be a guest on radio station Voice of Africa (VOA). VOA’s Vincent Makori interviewed me and asked for my thoughts on U.S. President Barak Obama’s new initiative to increase research to find a cure for HIV. Visit VOA here: http://www.voanews.com/section/africa/2204.html
UCL-Lancet Lecture 2013: “Charity Does No Rhythm With Development”
Published by UCL Lancet on November 13, 2013
On November 13, 2013, I was invited to give a UCL-Lancet 2013 lecture. In this presentation, I shared my perspective of Rwanda’s experience in mobilizing partnerships to help us achieve universal health coverage, with a social-entrepreneurship-business mindset. We discussed how open access research, “reverse innovation,” and equitable global partnerships rooted in solidarity can reinvigorate the pursuit of health for all.
Read more about the UCL-Lancet lecture and other presentations here:http://www.ucl.ac.uk/global-health/projectpages/symposia/Lancet_Lecture_2013
2013 Skoll World Forum: “Can It Be Replicated? A Look at Rwanda’s Development Gains in Context”
Published by Skoll on August 2, 2013
On August 2, 2013, I was invited to speak at the Skoll World Forum and present a discussion, “Can It Be Replicated? A Look at Rwanda’s Development Gains in Context.” I was joined by the following social entrepreneurs:
MARY ROBINSON, Former President of Ireland, President of Mary Robinson FoundationMary Robinson is President of the Mary Robinson Foundation — Climate Justice. She served as President of Ireland from 1990-1997 and UN High Commissioner for Human Rights from 1997-2002. She is a member of The Elders and the Club of Madrid, and is the recipient of numerous honours and awards, including the Presidential Medal of Freedom from the President of the United States, Barack Obama. Mary served as Founder and President of Realizing Rights from 2002-2010.
DALE DAWSON, Founder and, BRIDGE2RWANDA
Dale Dawson is Founder and CEO of Bridge2Rwanda, a social enterprise that facilitates business development in Rwanda and creates opportunity for Rwandan students to study abroad. He serves on President Paul Kagame’s Presidential Advisory Council and the Urwego Opportunity Bank, Rwanda’s largest micro-finance bank. In the first half of his career, Dale was an investment banker, entrepreneur and KPMG partner.
PAUL FARMER Co-Founder, Partners in Health
Paul Farmer, MD, PhD, is Kolokotrones University Professor and Chair of the Department of Global Health and Social Medicine at Harvard Medical School, Chief of the Division of Global Health Equity at Brigham and Women’s Hospital in Boston, and Co-Founder of Partners In Health. He also serves as UN Special Adviser to the Secretary-General on Community Based Medicine and Lessons from Haiti.
MATTHEW BISHOP, US Business Editor, The Economist
Matthew Bishop is the US Business Editor of The Economist.
He is the author of several books with Michael Green, including ‘Philanthrocapitalism: How Giving Can Save the World’, ‘The Road From Ruin’ and ‘In Gold We Trust? The Future of Money in an Age of Uncertainty’. Mr Bishop is also the author of ‘Essential Economics’. Mr. Bishop chaired the World Economic Forum’s Global Agenda Council on Philanthropy and Social Innovation, and was a member of the Advisors Group to the United Nations International Year of Microcredit in 2005
The Skoll World Forum on Social Entrepreneurship aims to “accelerate the impact of the world’s leading social entrepreneurs by uniting them with essential partners in a collaborative pursuit of learning, leverage and large scale social change.”
Learn more about the forum here: http://www.skollworldforum.org
The Skoll Foundation brings together social entrepreneurs and other innovators to solve pressing problems across the world. Learn more about the Skoll Foundation here: http://www.skollfoundation.org
International Society for Neglected Tropical Diseases Meeting
London, UK on July 15, 2013
On February 12, 2013 I spoke at the International Society for Neglected Tropical Diseases Meeting in London about the global healthcare implications of co-infections with NTDs and with other diseases. Watch videos of additional presentations here: http://www.isntd.org/#/isntd-coinfections/4573887174
Commenting on Lancet Publication “Redefining Global Health-Care Delivery:” Reflections On Global Health Delivery
Kigali, Rwanda on May 23, 2013
World Bank President Jim Yong Kim, Dr. Paul Farmer, and Professor Michael Porter recently published a paper in the Lancet, titled “Redefining global health-care delivery.” The publication, which analyzes health care delivery in the heart of the intersection of poverty and serious illness, can be found here: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2813%2961047-8/fulltext#article_upsell In this video, I offer my comments on my colleagues’ paper. This video was recorded by Daniel Murenzi.
Discussing the Importance of Priority Setting in Health
Kigali, Rwanda on May 1, 2013
In this video, filmed on May 1, 2013, I share my perspective on the importance of priority setting in health. Planning is an integral tool in any sector, and priorities and timelines must always be set in order to move forward effectively and efficiently.
2010 Global Burden of Disease Study: Country-Level Data Launch
Kigali, Rwanda on March 5, 2013
On March 5, 2013, the Institute of Health Metrics and Evaluation (IHME) in Seattle, Washington launched their data findings from the Global Burden of Disease (GBD) 2010 Study. The GBD Study is the largest and most comprehensive effort to date to measure epidemiological levels and trends worldwide. More than 1,000 GBD collaborators from 108 countries participated in the study. I strongly believe that health decisions must be evidence-based and driven by sound, culturally sensitive data. My Rwandan colleagues and I use the IHME’s GBD data often as we make our evidence-based data-driven decisions for the Health Sector. Learn more about the IHME, the GBD Study and to access data here: http://www.healthdata.org/gbd
Delivering Open Remarks at the Susan G. Komen International 2013 Global Women’s Cancer Summit
Washington, DC on February 19, 2013
On February 19, 2013, I was very honored to deliver the opening remarks at the Susan G. Komen International 2013 Global Women’s Cancer Summit in Washington, DC. This Summit brought together leaders from across the world to discuss the growing burden of women’s cancers, an important issue as we each face the growing burden of non-communicable disease on national levels. Learn more about the Susan G. Komen International Global Women’s Cancer Summit here: http://ww5.komen.org/News/Susan-G–Komen-for-the-Cure-Convenes-Global-Women-s-Cancer-Summit;-Worldwide-Collaboration-Aims-to-Tackle-Breast,-Cervical-Cancer.html
Presentation for the the International Society for Neglected Tropical Diseases Co-infections 2013 Meeting
London, UK, February 11, 2013 (Filmed in Kigali, Rwanda)
On February 12, 2013, I spoke at the International Society for Neglected Tropical Diseases (ISNTD) Coinfections Meeting, which took place at the Wellcome Trust in London, UK. This society aims to create multidisciplinary partnerships with NTD specialists, development professionals, research scientists, governments, donor & philanthropic organization and the private sector in order to improve healthcare outcomes globally.
Watch videos of additional presentations here: http://www.isntd.org/#/isntd-coinfections/4573887174
ISNTD Coinfections brings together experts in NTDs, other diseases and associated conditions of poverty – including HIV/AIDS, TB and malaria – who will be addressing the latest developments in these fields and their impact on NTD control with a view to effectively impacting poverty and development in the long-run. The Aim of this Coinfections group is to improve the delivery of healthcare and poverty alleviation among the most vulnerable by integrating resources across research, funding and advocacy with a focus on disease prevention and cure programmes.
Learn more about the International Society for Neglected Tropical Diseases here: http://www.isntd.org/
Learn more about the International Society for Neglected Tropical Diseases Coinfections group here:http://www.isntdcoinfections.com/
Presentation for 2013 GET-Health Summit
New York, NY, USA, February 7, 2013 (Filmed in Kigali, Rwanda)
On February 2013, I shared this video message at the Global Education and Technology (GET) Health Summit in New York City, hosted at the United Nations. My remarks were part of the Ministerial Forum and were shared on February 7th. The summit was convened by the Johns Hopkins Center for Clinical Global Health Education and by the Global Partnership Forum.
Learn more about the Global Education and Technology Health Summit here:http://www.ukcds.org.uk/news-events/events/global-education-technology-health-summit
Presentation for 6th World Congress on Pediatric Cardiology and Cardiac Surgery
Cape Town, South Africa Published: February 5, 2013 (Filmed in Kigali, Rwanda)
For the 6th World Congress on Pediatric Cardiology and Cardiac Surgery, that took place 17-22 February, I offered a video remarks. My presentation titled “Uniting to address pediatric cardiac disease in Africa: A message from Rwanda” provided insights into the principles leading health care delivery in Rwanda.
Presentation to US National FACE AIDS Leadership Summit
Boston, MA, September 30, 2012 (Filmed in Kigali, Rwanda)
On 30 September, I spoke to leaders of FACE AIDS student groups at universities across the US about the continued global activist movement to fight HIV/AIDS. FACE AIDS currently works in Rwanda (among many other countries) to build awareness among youth around prevention, care, and social support for HIV/AIDS.
Interview with Dr. Agnes Binagwaho
New York, NY, September 26, 2012 (Filmed in Kigali, Rwanda)
On 26 September, I spoke about the importance of participation, consensus, evidence-based health science, accountability, decentralisation and governance, and the role these factors have played in moving Rwanda forward.
A Talk for Harvard University’s Conference, “Universal Health Care: Challenges, Measurements, and Evaluation Strategies”
Boston, MA, September 13, 2012 (Filmed in Kigali, Rwanda)
On 13 September 2012, Harvard University hosted a conference on Universal Health Care. I participated via video-lecture and a video-Skype discussion with economists and public health professionals from around the world.
“The World is a Little Village”
Published by Dartmouth College, Hanover, NH on August 1, 2012
On 1 August 2012, I gave a brief interview on Rwanda’s new Human Resources for Health Program in collaboration with the consortium of universities in the United States.
“Time for a Paradigm Shift in Global Health: Equity, Science, Participation, Sustainability”
A talk with Dartmouth College, published on July 30, 2012
On 30 July 2012, I gave a public lecture in partnership with The Center for Health Care Delivery Science at Dartmouth College on how Rwanda’s experience can inform a paradigm shift in global health and why there is an urgent need for global solidarity.
Global Health Corps Fellows Orientation 2012
New Haven, CT, July 10, 2012
On Tuesday, 10 July 2012 I spoke via YouTube at the Orientation for the 2012-2013 Global Health Corps Fellows. This message can also can be applicable to students and young people interested in global health issues.
Wilton Park Conference: “The New Era in HIV/AIDS Treatment and Prevention: Science, Implementation and Finance”
Geneva, 27-28 June 2012
During the 2012 Wilton Park Conference titled “The new era in HIV/AIDS treatment and prevention: science, implementation and finance,” I spoke via YouTube with Dr. Sabin Nsanzimana, Head of the HIV/AIDS, STIs and Other Blood Borne Infections Division in the Rwanda Biomedical Center, on Rwanda’s country perspective on treatment as prevention for HIV.
Salzburg Global Seminar – Strengthening Leadership and Policy for Improving Care in Low and Middle Income Economies
Salzburg, Austria, 24 April 2012
This week, I spoke at the Salzburg Global Seminar on “Strengthening Leadership and Policy for Improving Care in Low and Middle Income Economies.” I was invited to speak on a panel during the seminar’s fourth day, and discussed improvements in system-wide procurement and infrastructure development as an example of Rwanda’s approach to quality improvement. You can view the video of my speech above, and a program description at the Salzburg Global Seminar website.
Harvard College Course Video Presentation: Health Systems Strengthening and Social Justice
Cambridge, Massachusetts, 22 November 2011
I delivered these remarks via Youtube for a course taught at Harvard College called “Case Studies in Global Health: Biosocial Perspectives.” This video presentation on Tuesday, 22 November 2011 was aired in conjunction with a lecture by Partners In Health – Rwanda Country Director, and Chair of the Rwanda Biomedical Center, Dr. Peter Drobac. My video presentation and Dr. Drobac’s lecture were accompanied by a discussion with Professors Paul Farmer and Arthur Kleinman.
Salzburg Global Seminar – Concluding Remarks
Salzburg, Austria, 30 September 2011

On the concluding day of the Salzburg Global Seminar: “Innovating for Value in Health Care: Better Cross-Border Learning, Adaptation, and Adoption,” I delivered remarks via teleconferencing technology.
Seeing and hearing the presentation and ideas on innovation delivered by the Salzburg participants on both individual and group levels throughout the week, I found the type of community created in such a short time to be one that has great potential to continue in several important ways.
In my remarks, I shared four key ideas on my perspective on the importance and concept of having a vision: (1) the creation of a vision, (2) the measurement of the progress to reach this vision, (3) the strategy in order to attain targets, and (4) the ability and prioritization of documenting the vision and the process taken to achieve. Every person and Health System must have a vision; we must know where we want to go. We need to know where we are now and how to get where we want to go in order to achieve our mission. We need to document how we did each step so that we can learn from our efforts.
The first part is the vision is identifying where we want to go, no matter whether other people find it too ambitious. It is our vision, and we need to stick to it. In doing so, we assure that all of our actions will be according to our own priorities. I believe that this vision must be shared because alone we cannot accomplish much. But when everyone is together, we can design together a national strategy and plan that is country-owned and community driven, because communities should be a part of the design from the beginning.
This participatory process brings together communities with the public and private sectors. It is then easy to be morally sound because, from the start, no one is left out and the vulnerable people are taken care of. This is the essential human rights concept behind access to care.
The second part of the vision is measurement – we need to effectively measure the health of our population, the quality of our health care system, our people’s to access to care and treatment, and the utilization of health services across our country. This is useful, on one hand to provide a baseline for evidence-based planning but also, on the other hand, to set targets according to the financial, human, and infrastructural resources that we have. This means that we can design results-oriented strategies and plans. If we do such assessment periodically, they will show us over time where we stand compared to our vision and our plan.
In my presentation, this brought me to the third category: how to reach our targets. We do this by designing good strategy, good action plans, and by creating good tools. We reach our targets by thinking outside of the box – with creativity, with flexibility, by learning as we are doing, and by being always being ready to question how we can do better. Innovation, of course, includes the pursuit of new partnerships, such as North-South partnerships like that between Dartmouth and Rwanda as well as South-South partnerships like that between Haiti and Rwanda.
The final fourth part of the vision is documentation of how we build our health sector. We need to learn from our progress and, more importantly, from our mistakes. To facilitate this learning, we need to conduct research for better policies, better strategies, and better ways to implement. This is implementation science, which teaches us to reduce to gap between what we know from clinical research and what we actually deliver to our population. Today, implementation science requires as much research as clinical science because improving policies, strategies, and delivery allows us to produce better health with the same resources. Sometimes, improvement of our strategies and implementation produces even greater results when it is about public health by teaching us how to bring things to scale using opportunities in a synergistic way that makes the money go farther. We need to see health care delivery as a social business where the units to produce are health, enjoying life, and wealth.
Friends, good intentions, innovations, creativity, flexibility, and clinical science are not enough because poor planning and bad procurement can undermine health just as much as bad will, business as usual, bad clinical services, and laziness. For example, in 2008 in Rwanda, we had an argument with the Global Fund on mosquito net procurement that delayed distribution for twelve months. Because we were not allowed to use the Global Fund money before an agreement was reached, we were obliged to redo the entire process. In the end, the money we received was the same, because we had been genuine and had indeed done the procurement honestly; yet as a result of this delay, Rwandans died of malaria. This can be understood by health care delivery science: the Global Fund should be held responsible for system outcomes in the same way that the health professional is held responsible for the death of patients because of his or her bad practice.
Another example is the bad decision not to vaccinate Haitians against cholera during the country’s cholera outbreak because the vaccine was said to be too expensive. This decision has cost thousands of Haitian lives. The development partners who made that decision should be held responsible for this, as it has cost the lives of innocent, vulnerable Haitian people. Health care delivery science teaches us how to attain the best outcomes with the resources we have while making us totally responsible for the principles upon which we implement and for the results that come from our actions.
Salzburg Global Seminar – From HIV to HPV
Salzburg, Austria, 27 September 2011

This week, I spoke at the Salzburg Global Seminar on “Innovating for Value in Health Care Delivery: Better Cross-Border Learning, Smarter Adaptation, and Adoption.” You can view the full program description here.
I was asked to present on Rwanda’s experience of integrating funding and programming for HIV into a comprehensive national strategic plan for quality basic health care. The talk was entitled: “From HIV to HPV: Same Principles in Building an Accessible, Affordable, and Equitable Health Care System in Rwanda.”
I started by discussing how, the week prior, I was in New York City for the United Nations High Level Meeting on Non-communicable diseases. It was intended to be a turning point in the global approach to tackling NCDs.
In that same UN hall, 10 years ago, we met to discuss how to make access to HIV prevention, care and treatment services a global priority. The 2001 UN summit on HIV/AIDS changed the conversation about HIV around the world.
At that time, we were told that we did not have the roads, the infrastructure, the cold chain, and the procurement capacity for drugs, consumable and reagents. We were told that we did not have the specialists, or even enough general practitioners and nurses, as many were killed during the 1994 Genocide Against the Tutsi. On top of all that, the so-called “experts” of health implementation said that our population was illiterate. They said that our people did not wear watches, so they could not read and know the time when they would have to take ARVs and could thus not adhere to therapy. They claimed that we should concentrate on prevention and not try to introduce ARVs to save the lives of those already infected, as it was too costly and dangerous for the health of the rest of the world –they expected our people would be non-adherent and said that this would create deadly resistance. But what they did not into account for was the cost of inaction, a cost that Rwanda would not tolerate.
Today, despite all of the barriers, we are proud to say we now have universal coverage for antiretroviral therapy and one of the lowest prevalence rates in Africa at 2.8%.
We are also proud to say that we just completed our second dose of the HPV vaccine for girls aged 11 in Rwanda through our national comprehensive cervical cancer prevention and screening program. The coverage rate was 95% for the first dose and 97.4% for the second.
These two achievements, scaling up access to HIV care and launching the developing world’s first national HPV vaccination program, are not unrelated. Rwanda was able to vaccinate all of its girls aged 11 against HPV because we have strategically built upon the foundation of advances made in HIV care and treatment, among other communicable diseases.
We moved from a destroyed health sector after the war and the genocide to tackling and managing HIV and other infectious diseases. We moved to tackle and manage non-communicable and chronic diseases while not dropping our advances in infectious disease control.
Health in Rwanda in general is understood as an important element of development. The HIV program needed to be coherent with the overall development vision of the country. And, just as our HIV plan, our overall health plan is evidence-based and results-oriented. The strategy of the health sector must follow national priorities and be linked to the national development vision (in Rwanda this is our Vision 2020 as well as our plan for the MDGs). The results must be monitored and used for planning and programming. Implementation and adaptation must be results-oriented.
When a massive influx of new HIV treatment resources was made available after years of effort by activists and people living with HIV around the world, we immediately made the choice to apply to access these funds. We used them to save the maximum number of lives in the most sustainable manner. This meant building a system that provided the best possible care for all Rwandans.
This was also a political choice, as it was rooted in the principle of assuring that the plan left no one out of the benefits. During our needs assessment in 2001, we realized that women use less health services than men. We acknowledged this disparity and the Government issued a Ministerial instruction to assure that if one member of a family is on ART there would be no additional cost for all additional members of the family to be put on treatment. A unit cost for the family with the objective to assure women and children access to prevention, care, and treatment was the first step in implementing an equitable health program based on gender, age and geographic equity. This is also why we made PMTCT the key family entry point to treatment.
Furthermore, we needed to assure in the beginning that people from higher socioeconomic levels would not be served more than poor, vulnerable patients, as we only had medicine for 3,500 people compared to the high volume of people in need of ARVs in order to survive. We assured this by putting civil society at the heart of the fight to regulate the selection of beneficiaries in health facilities. We also put civil society on the board of coordinating bodies for the fight against HIV. While we no longer face these problems today, as we currently have enough treatment for all, this principle still guides us to fight discrimination and segregation.
Our strategy is based on national ownership and responsibility. We have strong national leadership. In order for the government to be in the driver’s seat from A to Z, we coordinate our development partners in committees chaired by a Rwandan civil servant. We developed national tools, which meant developing a policy, a strategy, and a plan.
Our institutions are responsible for normative functions (e.g. clinical standards, site accreditation) on performance. These are results-based contracts that do not allow delay. Once this national framework was in place – development partners were, and are still today, given a framework to which they can integrate. Partners align their programs to the national plan. If they don’t want to align with our plan, they can go to another country. Parents are also asked to align with us and follow our lead around the location of their work. Many development partners come and want to be in the city, or they go to a country and want to be by the beach to do their work. We realized quickly that we needed to be careful about this type of coordination with partners as well.
To assure the alignment of partners, we needed a participatory process. Partners need to participate in the design of the policies, strategies, and plans. They also need to sign their commitment of clear actions to be taken to support the process and clear indicators to be rigorously evaluated over time. This has allowed us to succeed with innovative approaches, including our common basket of procurement for ARV and consumable procurement and activities.
We assure also an equitable geographic coverage through strong coordination of our partners and with the political will to move resources out from the capital city. Another strategy we promote to assist with equitable distribution of human resources is performance-based financing, which helps incentivize nurses and doctors to continue working in remote areas as well as to increase and maintain the quality of the care they provide.
The other tool developed was the community-based health insurance (called Mutuelles de Sante), which aids in eliminating financial barriers to basic health care. One pillar of our strategy is to provide systematic health insurance for civil servants through a program called RAMA. For the rest of the population, we began Mutuelles. This health insurance scheme aims to protect every Rwandan citizen from all common diseases. Since some very poor people cannot afford the 2 USD co-pay per year, there is also a free health insurance paid by the government for the poorest percentage of the population.
All this is done to protect people living with HIV, as well as those who are HIV free, against the most common diseases. It is not effective to save a child through antiretroviral therapy, costing more than one hundred dollars a year, and then to lose that same child to treat diarrhea or malaria, for lack of five dollars. It is also not right to improve only the life of a small portion of our people.
The government’s financial support for Mutuelles for the poorest people in the population provided the opportunity to show to those who have to pay for themselves, that the poorest people with Mutuelles have better access to care than them. The result is that, last year, 98% of Rwandans had health insurance. We created both the demand and a new mentality among the rural population, who saw people poorer than themselves having access to health care. It created a revolutionary demand for pre-payment in a country where paying prior to needing care no longer existed.
In the area of capacity building we accomplished many goals that improve the health of all Rwandans, including the training of health staff at different levels and the provision of solar panels, computers, ambulances to the health centres. “AIDS money” has allowed the country to train health workers and to improve overall care. We have used it to provide incentives to improve human resources, allowing health workers to serve the poor. When you train a lab technician for HIV testing, you also train him/her to test for syphilis, other diseases and even pregnancies. The lab infrastructure and microscope he uses serves all diseases. Almost half of HIV/AIDS funds in Rwanda were directed to strengthen the general health system and to support non-health, multi-sector development.
Plans need to be community-driven if we want to solve the real problems at the community level. Because HIV is a disease linked with poverty, integration of HIV and AIDS programs needs to be part of a larger strategy for economic development and poverty reduction for the achievement of MDGs. I believe that this notion of health as a basic right is critical, and that this right must be protected and promoted by everyone.
We must have zero tolerance for vertical programs. This means we must consider an individual as a whole, not tackling one disease but instead tackling all public health issues by using the same service structures for the same communities with the same health workers.
Here is a concrete example of how, with “AIDS exceptionalism,” we strengthened the entire health system: to provide ARV services, we need to be able to first test for VCT and PMTCT to know if a person or pregnant women is HIV-positive. That means we need a laboratory for the testing. Before building or improving an existing laboratory, we need to provide common basic care to the clients of the sites where HIV treatment will be given. That means basic care for all, not only for PLWHA, and there is no site aimed only at HIV but, rather, aimed at comprehensive health facilities that treat the entire population for all diseases. Integration of HIV services in the health system is a prerequisite to provide ARVs in a safe manner while taking into consideration the needs of the entire population.
In Rwanda, we managed to use the influx of AIDS money to strengthen all sectors of the health system. We know that HIV is a cross-cutting issue. Within the health sector, AIDS money was used to rehabilitate or build infrastructures from scratch, such as health centers, delivery wards, laboratories, and consultation facilities. We have bought materials for communications, including telephones, computers, and ambulances.
Another key requirement for building a system is ensuring accountability from both sides, including countries and donors, through enforcement of transparency and anti-corruption measures. The greatest challenge that Rwanda and many other African countries face is that the health sector is largely externally financed. We have solved that partially by making the funds country-driven and directed them to meet community-defined needs.
However, many interventions remain under-funded, such as programs to address the link between food insecurity and health. Sustainability issues for interventions like ARV therapy remain beyond the financial means of most developing countries. We face the challenge of maintaining balance between our investments, by addressing the human resources deficit, while providing necessary services today. Development requires long-term support, and we face difficulties in firming up long-term donor commitments to projects focused on health systems strengthening. Partners must bring a spirit to plan for achievement and results, not simply a limited and arbitrary timeframe – what is not achieved in a sustainable way it will be lost one day.
While we face significant challenges, we also have a lot of opportunities. These include clear political and technical vision, strong government leadership, broad community and civil society participation, goodwill from all partners that results in global solidarity put into action, strong foundational programs on which to build, and motivated teams of health workers with the right skills.
By dedicating ourselves to making the new resources for HIV work to meet our vision, we have seen remarkable progress in the health of our population. Over the last five years, malaria morbidity has been reduced by 60% and under-five mortality has dropped by 50%. We have increased the proportion of infants receiving all basic WHO recommended immunizations from 75% to over 90%. Maternal mortality has dropped by nearly two-thirds. 98% of Rwanda’s 11 million people have health insurance. We have 45,000 community health workers and have successfully implemented our performance-based approach in the health sector.
So, on the shoulders of these advancements, we decided to tackle non-communicable diseases, which we saw as an important investment. The fight needed to start somewhere, and it is clear that for women we can mitigate cervical cancer with a vaccine, and breast cancer with self-detection or clinical detection. This is the place our government wanted to start. So on April 26th and 27th of 2011, 128,000 young Rwandan girls received their first shot of Gardasil – with no out-of-pocket payment – and Rwanda became the world’s first low-income country with a national HPV vaccine program.
Several early decisions were crucial to the success of our HPV vaccine initiative. First, we decided to vaccinate the girls at age 11, because at this age they are ready to receive and understand messages on reproductive health. We decided to vaccinate them in schools because 96% of girls in Rwanda go to school. Accordingly, we decided to widen our technical working group on vaccinations to include the Ministries of Education and Gender and Family Promotion, the Center for Treatment and Research on AIDS, Tuberculosis, Malaria, and Other Epidemics (TRAC Plus), and health workers engaged in the provision of cancer care. At the same time, throughout Rwanda, a sensitization campaign was done months in advance of the HPV vaccination. Many were involved in this, including health care professionals, local government officials, clergy, and the First Lady.
Second, the committee decided on a multi-phased vaccination strategy spanning three years. It started for girls in primary 6. After this first year, we planned to have two years of vaccinating girls in the second year of secondary school to assure that all girls aged 14 are vaccinated. After the third year, we planned to continue to vaccinate only in primary 6.
Looking at the central considerations of our decision to roll out the HPV vaccine, it is clear that an effective HPV vaccine program has to build on a national vaccination program. The HPV vaccine in Rwanda is also based on public-private partnership with Merck, which we see in reality as a public-private-community partnership, since our community health workers have helped us to identify the children that were not at school on the day of the vaccine. When you vaccinate at school, universal access to education is key to health equity.
I should note that the same accusations made against antiretroviral therapy and MDR-TB, as Jim Kim and Jaime Bayona have publicly spoken about, were raised against our HPV vaccine program. Researchers said that it was too expensive for Africa and that the HPV vaccine would take away from other vaccination programs (which already have nearly universal coverage in Rwanda). Also, they alleged that Africa’s high HIV prevalence would make the vaccine dangerous. But what they did not consider again was the cost of inaction and the danger to women, who would die of cervical cancer without the vaccine. Rwanda and its health sector leaders would not tolerate this cost.
The HPV vaccine in Rwanda relied heavily on government leadership and support, as well as a community health system that reaches all rural and urban persons. To provide timely, quality services without stock-out, the supply chain, distribution systems and cold chain have to be in place and monitored extremely carefully.
Integration was, and is, key to our approach to non-communicable diseases. Detection should be integrated with family planning, with life skills, and with economic development. The point is to be cost-effective while providing health care in an equitable manner that ensures accessibility and affordability to all individuals.
Historically, there has always been a 15-20 year lag between the introduction of a vaccine in rich and poor countries. But in Rwanda, thanks to the good partnerships we have and our human rights-based approach to development, we shortened that lag time in delivering the HPV vaccine to less than 2 years. This is something that can and should be done in many other poor countries – those who bear the brunt of the burden of disease are generally the last beneficiaries of advances in science and medicine.
Rwanda’s richest resource is its population. For this reason, all of the policies and strategies in our health sector are rooted in the pursuit of health equity and social justice. These advances in combatting communicable diseases and strengthening the health system have led to increased life expectancy, which now exceeds 50 years, leading to our people living longer and now showing an increased prevalence of NCDs later in life. This is an opportunity and a challenge, reflecting both our progress and the immense mountains we still have to climb to provide the necessary new services to our population.
Fighting diseases needs to start by good policies, strategies, and plans and needs to be integrated across sectors with the goal of strengthening the entire health system.
Global Health Principles: A focus on Health System Strengthening
Cambridge, April 7, 2011

This talk was given to undergraduates and graduate students at Harvard University, and hosted by the Harvard Institute for Global Health in Cambridge, MA. Prior to a Question and Answer session, I spoke to the students about how it is important to develop a health care system based around national programs and ownership. I discussed the example of HIV programs, the fight against cancer, care of people living with handicaps, and issues of human resources for health including professionals and community health workers. Students posed terrific questions about accountability, national ownership and challenges to scale-up.
Global Health Financing, Panel at Harvard Kennedy School
Cambridge, April, 7, 2011

A panel hosted by the Harvard Kennedy School; the Program in Global Public Policy and Social Change, in the Department of Global Health and Social Medicine of Harvard Medical School; the François-Xavier Bagnoud Center for Health and Human Rights, of Harvard University; and Partners In Health. Several panelists participated in a discussion concerning the payment for health services and access to essential services in resource-limited settings. Dr. Binagwaho spoke on the panel with other scholars including Paul Farmer, Kolokotrones University Professor, Harvard University; Cristian Baeza, Director for Health, Nutrition and Population, Human Development Network, World Bank; Robert Yates, Senior Health Advisor, DFID; and S.A.S. Kargbo, the Director of Reproductive and Child Health in the Ministry of Health in Sierra Leone. Each explained different models of health care financing and payment for services in various countries in Africa and other parts of the world. Dr. Binagwaho insisted on home grown solutions to payment schemes and on the sustainability of financing. After the panelists shared their views on payment for health care (e.g. individual payer, insurance provider, government as the payer), there was a designated period of Question and Answer with the audience. To conclude the event, the panelists agreed on the need for universal access to basic care with a shared understanding of health care as a human right.
Innovations to Improve the Quality of Health Care in Resource-Limited Settings
Lecture given in Boston, MA on 31 March 2011 on Innovations to Improve the Quality of Health Care

This lecture concerned innovations to advance the quality of health care in resource-limited settings with a focus on current programs and projected opportunities for improvement. In order to reach the Millennium Development Goals, especially those for health, countries must invest in innovations – both technological and political. We must agree that the responsibility to provide health care belongs to all people including the Government, the private sector and the general population. Improving access to prevention, care and treatment especially for those who are most vulnerable such as women and children, we need to have targeted innovative actions. Generally speaking, the world has come far since the MDGs were set in 2000. And yet we have a big push ahead of us. In order to advance as quickly as we need to – a big shift toward technology and communication must be made.
If health care is taken as a basic human right – something I believe strongly – these innovations must reach all persons within a country, with a focus on those who are most vulnerable. In Rwanda, there are four examples of such innovation: (1) the new non-surgical male circumcision device that does not require a sterile environment, PrePex; (2) the alert system called Rapid SMS whereby community health workers can alert the district and central levels of, for example, a woman who needs an ambulance to take her to the hospital to give birth simply by sending an SMS; (3) mUbuzima, another cell phone technology that allows the community to send a set series of indicators on the MDGs within their communities; (4) and the system of governance in Rwanda wherein the population is given a strong voice in policy, action and major decisions.
With innovative tools and new ways of managing them with enhanced ownership and accountability, countries will be able to accelerate providing access to health services for all.
The Cycle of Poverty and HIV Infection
Boston, July 8, 2011

This lecture explores the role poverty plays in preventing access to health care and discusses the vicious cycle of poverty and HIV infection. This is well illustrated by maps by of HIV distribution and poverty distribution worldwide.
Countries have to break the cycle of disease and poverty in order to achieve good health. The fight against HIV is one of the clearest examples of how the lack of access to care and treatment is a death sentence for the poor. And, beyond the affects of HIV/AIDS, a poor country in sub-Saharan Africa will not be able to reach development goals efficaciously without addressing the burden of other infectious diseases like malaria. Malaria claims millions of deaths in addition to debilitating tens of millions through chronic anemia. There is a need to promote prevention and, at the same time, improve case finding and treatment at the community level. This will lower the number of patients hospitalized for malaria and thus lower absenteeism among workers and students.
To fight HIV infection and malaria we need to link improvement in both prevention and care. We have to avoid choosing between one approach or the other given that both prevention and care are vital.Why does Africa face the vicious cycle of disease? By losing skilled people due to diseases, including doctors and nurses, rates of death among the population from other common diseases will rise since fewer professionals would be there to treat them.
In hospitals, beds occupied by those suffering from HIV-related diseases are limiting the space for patients sick with other treatable diseases. Thus, we see that AIDS kills even non-HIV infected patients because of lack of heath practitioners and lack of hospital spaces. In the education sector, the lack of teachers decreases the quality of education for the next generation (and a loss of investment for governments that have disbursed funds to trained teachers).
Most importantly, parents are dying in their productive and reproductive years and leaving orphans behind. As it is in the tradition, extended families and communities struggle to absorb these orphans. The times there have been no parents left and children without adults alive at home struggled to organize themselves into new families. But extended families, and even moreso child-headed households, cannot afford school and health care for their children, brothers, and sisters without solidarity—locally and nationally and internationally. The orphaning of all of these children makes people even poorer and more vulnerable. Without appropriate action we have feared that Africa would become more and more poor, with diminished capacity to defeat poverty.
So, thinking beyond the examples of AIDS and malaria, what is needed to break the cycle of disease and poverty? Good health increases production capacity, which in turn leads to economic growth and poverty reduction. This leads to better health for the overall population as they have more money to pay for health services.
Taking examples of Rwanda, this lecture indicated the importance of developing a national policy framework, coordinating partners, proactively promoting gender-equity, mobilizing funds, integrating vertical programs in public health facilities, assuring sustainability and breaking down geographic and financial barriers.
We cannot ensure the basic human right of access to care for all without this battle. In breaking the vicious cycle of poverty, no one is exempt: no government, no sector, no agency, no NGO, no part of civil society, no multilateral organization, no individual – no expert, no scientist, no public health professional. All must join the fight.
Health and Human Rights: Creating an Open Forum to advance Global Health and Social Justice
September 17, 2008
HumanRights Journal Launch, Here the link: – Part 1
HumanRights Journal Launch, Here the link: Part 2
The Right to Health and the Right to Information are linked. Open Access Journals are good entry point to access to information and improve access to health care.
Rwanda’s history, and particularly, before 1994, the role of state-controlled radio stations in the genocide, had demonstrated that the right to information was critical to protecting individuals. The Rwandan government sees Information and Communication Technology as a top priority, and is working tirelessly to increase Internet access nationally.
This lecture reflected also on the irony of research done in developing countries that can’t never been available to the study subjects, without them paying for it. This is why the efforts of open access Journal in promoting access to a wider audience should be applauded as it increases access to education, information, and health all necessary for fighting against the cycle of poverty.